Got a borderline ECG result and feeling a bit lost? Don’t worry, many people get these results, and it’s understandable to feel anxious. This guide is here to help, whether you’re a patient, doctor, or work with ECG machines. We’ll break down what a borderline ECG (electrocardiogram) means, why it happens, and your next steps, offering practical steps for patients, expert tips for healthcare professionals, and ways to improve ECG machine technology. For more information on next steps, see this helpful guide: Next Steps. Let’s figure this out together!
Navigating Borderline ECG Results: Essential Guidance
A borderline ECG result can be unsettling, but it doesn’t automatically mean something’s seriously wrong. It warrants a closer look, signaling the need to investigate possible heart abnormalities. Many factors can cause a borderline result – stress, dehydration, or even a tiny error during the test. The key is to determine why you have this result to maintain cardiovascular health. Think of it as a yellow light, not a red one.
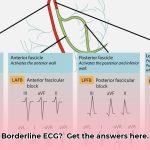
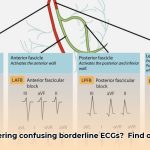
Decoding the ECG Report: What Does “Borderline” Really Mean?
Your electrocardiogram (ECG) measures your heart’s rhythm and electrical activity. A “borderline” result simply means the ECG detected some minor irregularities that don’t immediately point to a serious heart problem but are unusual enough to require further investigation. Some common reasons for borderline ECG findings include temporary issues like stress or medication side effects, and technical factors. However, it’s crucial to rule out any underlying heart conditions, which is why further evaluation is important for diagnostic accuracy.
Here’s a more detailed breakdown of potential causes:
- Temporary Issues: Stress, dehydration, anxiety, excessive caffeine intake, nicotine use, or even not enough sleep can temporarily affect your heart rhythm and blood pressure. These factors can disrupt the delicate balance of electrolytes and hormones that regulate heart function.
- Medication Side Effects: Certain medications, including some antidepressants, antihistamines, and decongestants, can influence your heart’s electrical activity and heart rate variability. It’s important to provide your doctor with a complete list of medications you’re taking.
- Technical Factors: Sometimes, a tiny movement during the test, a slight problem with electrode placement, or electrical interference from other devices can create a borderline result, affecting the ECG interpretation. Properly calibrated equipment and trained technicians are essential for accurate results.
- Normal Variations: It’s important to remember that what’s considered “normal” can vary slightly from person to person. Some individuals may naturally have minor variations in their heart’s electrical activity that don’t indicate any underlying health problem.
- Underlying Conditions: While less common, a borderline ECG may indicate an underlying heart condition, such as a minor arrhythmia (irregular heartbeat), coronary artery disease, or even a thyroid problem.
What to Do if Your ECG is Borderline: Your Next Steps
Your doctor is your best resource in understanding and managing borderline ECG results. Here’s what you should do to ensure proper cardiac monitoring:
- Schedule a follow-up appointment promptly. Don’t delay; this allows your doctor to review your results in detail, consider your overall health picture, and advise on the next steps for cardiac risk assessment. Ideally, schedule the appointment within a week or two of receiving your results.
- Be prepared to discuss your lifestyle. Your doctor will want to know about your daily habits and lifestyle modifications: diet (including sodium and fat intake), exercise, stress levels, amount of sleep, and if you consume caffeine or alcohol. Be honest and provide as much detail as possible.
- Report any symptoms, no matter how small. Even seemingly insignificant details – such as chest pressure you notice only occasionally, a slightly faster heartbeat, occasional shortness of breath, dizziness, or fatigue – could be important clues that may indicate arrhythmia or other heart problems.
- Ask questions. Don’t hesitate to ask your doctor to explain anything that’s unclear regarding your cardiovascular risk factors. Some good questions to ask include: “What specific abnormalities did the ECG detect?”, “What are the potential causes of these abnormalities?”, “What further tests do you recommend, and why?”, and “What lifestyle changes can I make to improve my heart health?”.
A Closer Look for Healthcare Professionals: Interpreting Borderline ECGs
Doctors and cardiologists deal with borderline ECG results frequently and understand the nuances involved. Interpreting these findings requires careful consideration of several factors:
- Patient’s Medical History: Existing conditions (diabetes, hypertension, thyroid disorders), medications (including over-the-counter drugs and supplements), family history of heart problems (especially sudden cardiac death or arrhythmias), and overall health play a critical role in ECG interpretation for patients’ health outcomes.
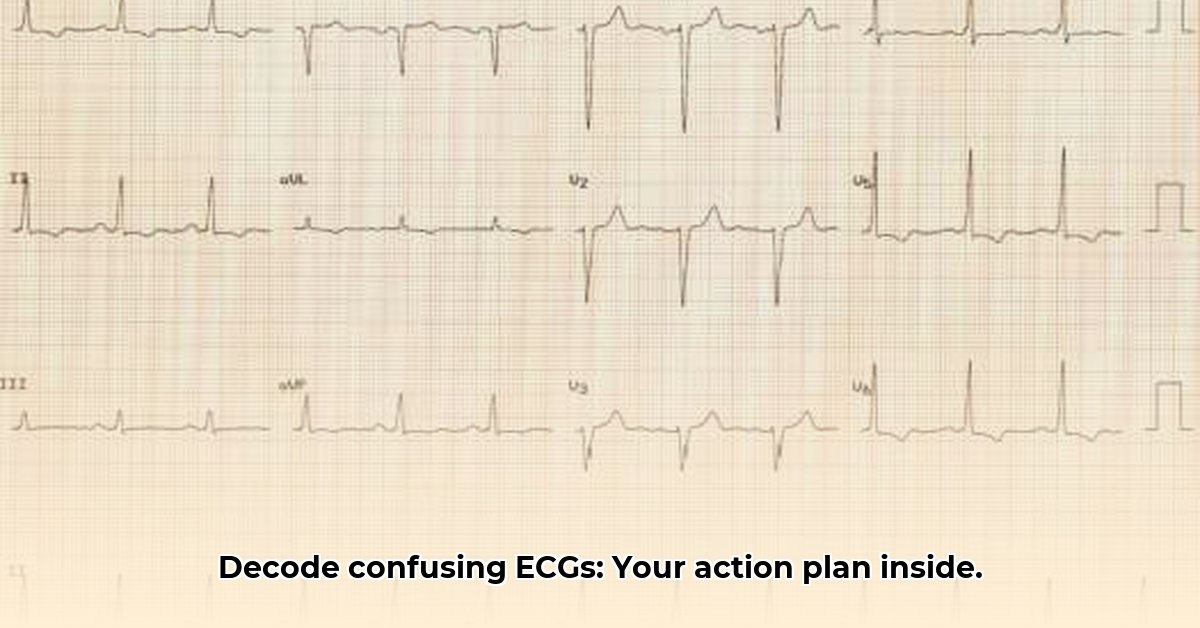
- Thorough ECG Analysis: Your doctor will meticulously examine the entire ECG waveform, paying close attention to subtle changes in different parts of the tracing to detect any consistent rhythms. They’ll look at the P wave, QRS complex, ST segment, and T wave, noting any deviations from the norm.
- Additional Testing: Depending on the findings, additional tests might be recommended, such as a Holter monitor (to record heart activity over 24-48 hours), an echocardiogram (ultrasound of the heart), blood tests (to check electrolyte levels, thyroid function, and cardiac enzymes), or a stress test (to evaluate heart function during exercise).
- Risk Assessment: Your doctor will consider all available information to determine your overall risk of heart problems. This helps them decide on the most appropriate course of action to improve patient care. They may use risk scores or algorithms to estimate the likelihood of future cardiac events.
Improving ECG Technology: The Manufacturer’s Role
ECG device manufacturers are constantly working to improve the accuracy and clarity of ECG interpretations. This involves refining signal processing, enhancing noise reduction algorithms, implementing advanced filtering techniques, harnessing machine learning and developing user-friendly interfaces for healthcare technology. The goal is to provide healthcare professionals and patients with more reliable and easily understandable ECG reports, ultimately leading to faster and more accurate diagnoses.
Specific areas of improvement include:
- AI-powered Interpretation: Artificial intelligence can be used to analyze ECG waveforms with greater precision than humans, identifying subtle patterns that might be missed. AI can also help to differentiate between normal variations and true abnormalities.
- Wireless Monitoring: Wireless ECG devices allow for continuous monitoring of heart activity in a variety of settings, providing a more comprehensive picture of heart function than a single snapshot in time.
- Improved Electrode Technology: Advances in electrode design can improve skin contact and reduce artifact, leading to more accurate ECG readings.
- Data Integration: Integrating ECG data with other patient information, such as electronic health records and wearable sensor data, can provide a more holistic view of a patient’s health.
The goal is to provide healthcare professionals and patients with more reliable and easily understandable ECG reports, ultimately leading to faster and more accurate diagnoses.
Frequently Asked Questions (FAQs)
Q: Is a borderline ECG result always serious?
A: No, not necessarily. Many factors can lead to borderline findings. However, a follow-up is always needed to rule out any underlying conditions. It’s a signal to investigate further, not a definitive diagnosis.
Q: What if my doctor wants more testing?
A: Trust your doctor’s judgment. These tests offer valuable information and are designed to help ensure your heart health. They are not meant to cause anxiety, but to provide clarity.
Q: How can I improve my heart health?
A: A heart-healthy lifestyle is crucial: regular exercise (at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity exercise per week), a balanced diet (rich in fruits, vegetables, and whole grains), managing stress (through techniques like meditation or yoga), and avoiding smoking all contribute significantly to a strong heart. Also, maintain a healthy weight and get adequate sleep (7-8 hours per night).
Remember, it’s simply a call for a more thorough investigation. With a comprehensive evaluation and appropriate follow-up care, both you and your healthcare provider can determine the next steps to improve your heart health.
Tailoring Borderline ECG Interpretation Across Age Groups
Key Takeaways:
- A borderline ECG isn’t necessarily a cause for panic, but it does require further investigation for cardiac health. It requires a detailed approach rather than immediate alarm.
- Factors like technical errors, lifestyle choices, and underlying conditions can influence results found in clinical cardiology, making a comprehensive evaluation essential.
- Age significantly impacts ECG interpretation; what’s normal for a young adult might be concerning in an older person, influencing cardiac outcomes. Always consider the patient’s age and overall health status.
- Immediate medical attention is warranted if you experience symptoms alongside a borderline ECG to prevent cardiac events. Symptoms such as chest pain, shortness of breath, dizziness, or palpitations should never be ignored.
- Follow-up appointments, lifestyle adjustments, and further testing are often recommended for preventive cardiology measures. These steps are crucial for early detection and management of potential heart problems.
- Healthcare professionals play a crucial role in interpreting results accurately and guiding appropriate follow-up care to provide quality care. Their expertise is essential for ensuring optimal patient outcomes.
Understanding Borderline ECGs
Think of an ECG as a snapshot of your heart’s electrical activity. A borderline ECG is like a slightly blurry photo requiring a closer look for improving cardiovascular outcomes. These inconclusive findings don’t automatically signal a heart problem, but
- Wellness Fair Ideas for Work to Boost Employee Wellbeing - December 15, 2025
- Affordable Employee Wellness Fair Ideas for Any Budget - December 14, 2025
- Employee Wellness Programs Strategically Benefit Employee Health And Retention - December 13, 2025