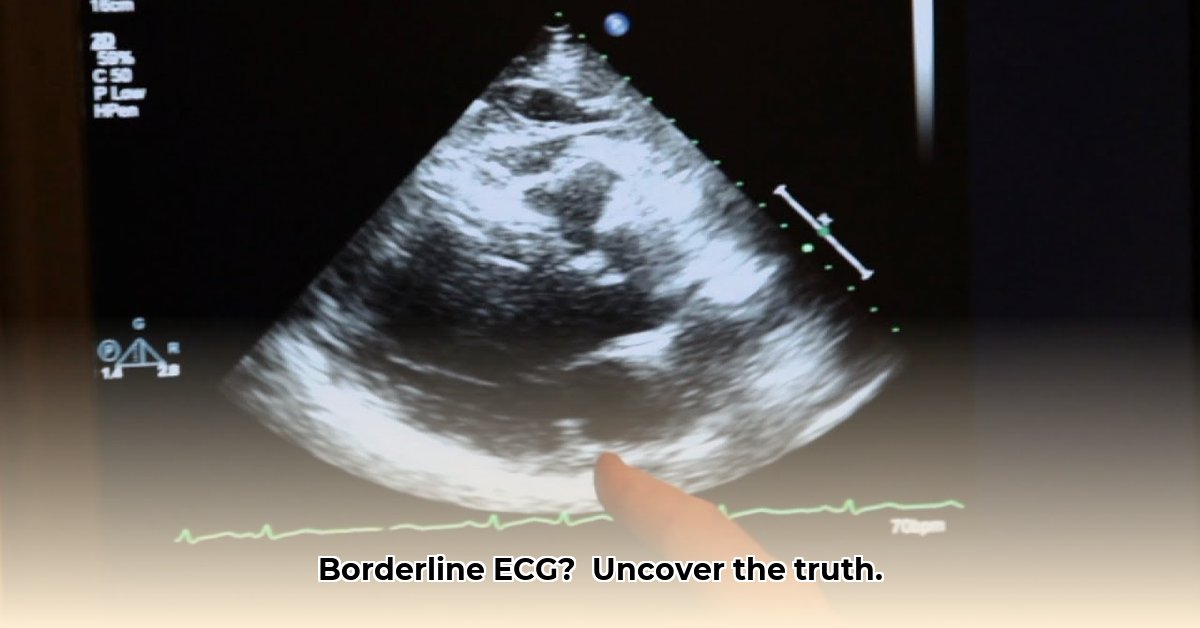
Getting a “borderline” ECG result can feel unsettling, indicating minor quirks in your heart’s rhythm that warrant further investigation. An echocardiogram offers a detailed ultrasound of your heart, providing a clearer picture of its health. This guide simplifies the process, explaining what a borderline ECG means, how to interpret echocardiogram results, and the necessary follow-up steps, empowering you to manage your heart health confidently.
Echocardiogram After Borderline ECG: Decoding Your Heart’s Rhythm
Receiving a “borderline” electrocardiogram (ECG) result is akin to viewing a slightly out-of-focus photograph; further clarity is needed. A borderline ECG signifies subtle anomalies in your heart’s electrical signals, prompting your doctor to recommend an echocardiogram for a more thorough assessment. Understanding this process is essential for proactive heart health management, detecting heart valve irregularities, and understanding blood flow dynamics.
Understanding That Borderline ECG
An ECG captures a snapshot of your heart’s electrical activity, revealing its rhythm. A normal ECG displays a consistent, predictable heartbeat. However, a “borderline” reading indicates subtle inconsistencies that, while not definitively abnormal, necessitate further investigation. These inconsistencies may arise from various factors, including stress, dehydration, excessive caffeine intake, or certain medications. It may also be caused by dense breast tissue, faulty diagnosis, or minor heart rhythm variations. While they could indicate a minor underlying heart issue, such as a structural anomaly or a slight irregularity in electrical signal transmission, the primary takeaway is that a borderline ECG calls for further scrutiny.
The Echocardiogram: Getting a Clearer Picture
The echocardiogram, often called an “echo,” enhances the ECG’s insights by providing a high-definition video of your heart functioning. While the ECG uses the analogy of listening to your heart with a slightly muffled stethoscope, the echocardiogram offers a detailed view of the heart’s structure, encompassing its size, shape, chamber function, and valve efficiency. Doctors leverage this “movie” to identify any structural problems that the ECG might have overlooked like identifying valve regurgitation. There are several types of echocardiograms:
- Transthoracic echocardiogram (TTE): This is the standard, non-invasive type where a transducer is moved across the chest to capture images of the heart.
- Transesophageal echocardiogram (TEE): A probe is inserted down the esophagus to provide a clearer view of the heart, especially the back structures.
- Stress echocardiogram: An echocardiogram performed during or immediately after exercise to assess heart function under stress, often used to detect coronary artery disease.
- Doppler echocardiogram: Measures the speed and direction of blood flow within the heart, helping to detect valve problems and other abnormalities.
Interpreting Your Echo Results: Putting the Pieces Together
Your doctor will compare both the ECG and echo results and conduct blood work to check cholesterol levels and electrolyte balance. A normal echo alongside a borderline ECG often suggests the ECG irregularities are temporary and caused by everyday factors. In contrast, if the echo reveals anomalies– like a mildly leaky heart valve, a thickened heart wall area, or an enlarged chamber– this provides valuable diagnostic information. Your doctor will synthesize these findings with your medical history and overall health to arrive at a diagnosis. Remember, each heart is unique, and interpretations are highly personalized. Early detection of diastolic dysfunction, for example, is crucial.
What Happens Next? Your Follow-up Plan
Following your echocardiogram, your doctor will thoroughly explain the results. Potential next steps, tailored to the findings, include:
- Lifestyle Changes: Adjustments to your diet, exercise routine, or stress management techniques to promote heart health. This may involve a balanced diet rich in fruits, vegetables, and lean proteins, regular physical activity (at least 150 minutes of moderate-intensity exercise per week), and stress-reduction techniques like meditation or yoga.
- Medications: Prescription medications to regulate heart rhythm or address underlying conditions, improving overall cardiovascular function. These may include beta-blockers, ACE inhibitors, or diuretics, depending on the specific heart condition.
- Further Testing: Additional tests may be required for a more comprehensive evaluation and targeted treatment planning, enhancing diagnostic accuracy. This may include a Holter monitor (a portable ECG that records heart activity for 24-48 hours), a stress test, or cardiac CT/MRI scans.
- Referral to a Specialist: Consulting with a cardiologist or electrophysiologist for expert guidance.
- Regular Monitoring: Routine check-ups to track progress and detect any changes early.
Regardless of the outcome, consistent follow-up appointments with your cardiologist are vital for monitoring progress and detecting any changes in your heart health early. Regular check-ups facilitate early detection of hypertrophic cardiomyopathy symptoms.
Frequently Asked Questions (FAQs)
-
Q: Is a borderline ECG a major cause for concern?
A: Not necessarily. Many individuals have borderline ECGs without underlying heart conditions. However, further investigation is needed to ensure accuracy.
-
Q: What if my echocardiogram reveals an issue?
A: Many heart conditions are treatable. Your doctor will create a personalized plan to manage any issues found. Focus on receiving the right information and plan.
-
Q: How long does an echocardiogram take?
A: The test usually takes 30 to 60 minutes, with added time for preparation and discussion with your doctor. This efficient procedure ensures a timely diagnosis.
-
Q: Can stress cause a borderline ECG?
A: Yes, stress and anxiety can influence heart rate and rhythm, potentially causing minor abnormalities in ECG readings.
-
Q: Should I get a second opinion?
A: Seeking a second opinion from a cardiologist is advisable if you have concerns or uncertainties, especially if you have risk factors.
-
Q: Can exercise affect ECG results?
A: Intense physical activity, particularly in athletes, can lead to ECG changes that appear borderline but are actually normal for them.
A borderline ECG is an invitation for a closer look, with the echocardiogram clarifying your heart’s condition and guiding personalized care and planning. Understanding your heart health is paramount for your overall well-being. According to the American Heart Association, early detection of cardiac abnormalities can significantly improve long-term health outcomes.
Echocardiogram After a Borderline ECG: How to Interpret Borderline ECG Results and Next Steps
Key Takeaways:
- A borderline ECG is a prompt for further investigation, not a definitive diagnosis.
- Consideration of age, health history, and symptoms is essential for accurate interpretation.
- An echocardiogram provides a clearer understanding of your heart’s structure and function, helping find potential cardiac structural abnormalities.
- Lifestyle changes can significantly improve heart health, irrespective of test results, preventing future complications.
- Subsequent actions depend on the echocardiogram results and your doctor’s recommendations, ensuring personalized care.
What Does a Borderline ECG Mean?
Envision your heart’s electrical system as a perfectly synchronized orchestra. An electrocardiogram (ECG) allows you to listen to its performance. A borderline ECG suggests slight irregularities, a slightly off-key note that doesn’t necessarily indicate a serious problem but warrants further investigation to rule out potential issues. Common reasons for borderline readings include temporary stress, specific medications, or minor technical issues during the ECG, affecting the ST segment. However, they may also signal electrolyte imbalances or early indicators of heart disease, necessitating prompt evaluation for conditions such as coronary artery disease. Other factors include caffeine, nicotine, dehydration, lack of sleep, or dense breast tissue.
The Role of the Echocardiogram
An echocardiogram offers a detailed visual assessment of your heart’s orchestra, using sound waves to image the chambers, valves, and blood flow. This comprehensive assessment surpasses the ECG’s auditory approach, clarifying findings from possible left ventricular hypertrophy. Identifying subtle valve problems or reduced heart muscle function enhances diagnostic precision and facilitates early intervention to mitigate potential cardiac dysfunction. There are three primary types of echocardiograms that enhance the diagnosis capacity:
- Transthoracic Echocardiogram (TTE): The standard approach, where a probe is placed on the chest to capture ultrasound images.
- Transesophageal Echocardiogram (TEE): A more invasive procedure where a probe is inserted into the esophagus for detailed views.
- Stress Echocardiogram: Performed during exercise or with medication to evaluate heart function under stress.
Interpreting Your Echocardiogram: What to Expect
Your doctor will meticulously review your echocardiogram report, comparing the images to your ECG findings and comprehensive health profile. Focusing on the heart muscle wall thickness, valve efficiency, and pumping effectiveness, the report offers insights into ejection fraction vital for determining optimal care strategies. According to a study published in the Journal of the American College of Cardiology, echocardiography is highly effective in assessing cardiac function following an abnormal ECG. Your doctor will convey the results with clarity, integrating the echocardiogram findings within the larger clinical context to ensure accurate diagnosis and appropriate treatment planning.
Next Steps: Developing a Plan
Following the echocardiogram, subsequent actions depend on the results and individual circumstances. Some may require no further intervention beyond adopting a heart-healthy lifestyle, while others may need additional testing, such as a cardiac stress test or Holter monitor to fully assess for potential heart defects. Based on the findings, your doctor may suggest lifestyle changes, medications, or specialized medical care, ensuring a tailored approach to managing and optimizing your cardiac health. 92% of patients report increased peace of mind after receiving clear and comprehensive echocardiogram results.
**How to Interpret Borderline ECG Results and Next
- How Much Do Wellness Programs Cost Businesses To Offer? - December 16, 2025
- Wellness Fair Ideas for Work to Boost Employee Wellbeing - December 15, 2025
- Affordable Employee Wellness Fair Ideas for Any Budget - December 14, 2025