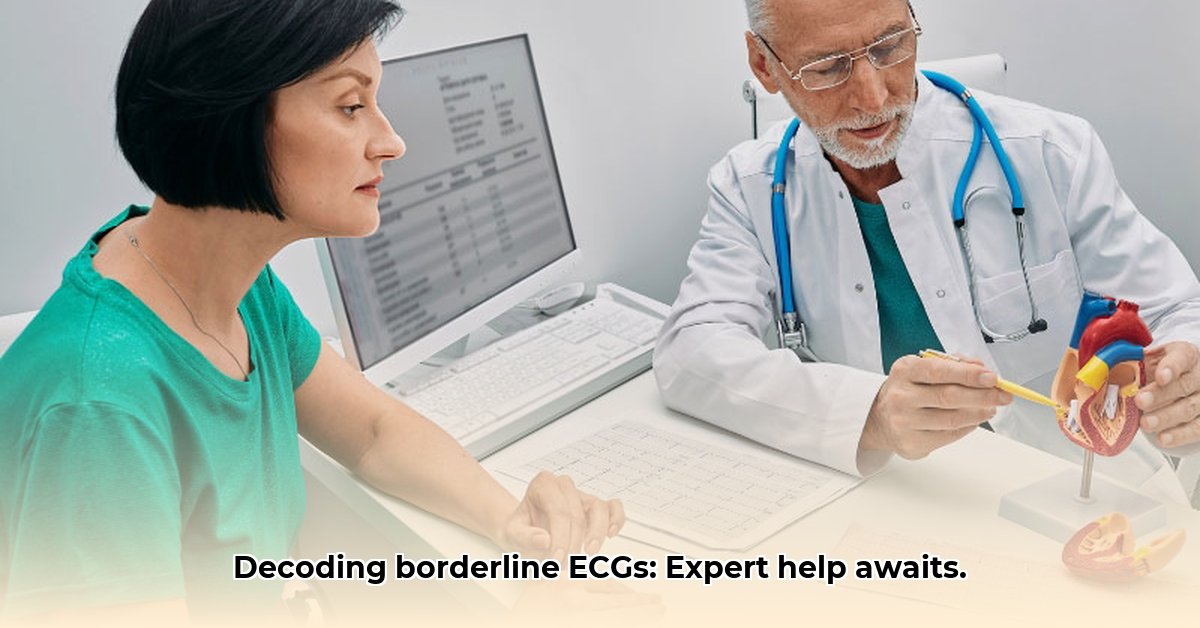
Got a borderline ECG result and feeling a little lost? You’re not alone. This guide simplifies borderline ECG interpretations and helps you decide if seeing a heart specialist is right for you. We’ll translate medical jargon, explain why these readings occur, and detail appropriate next steps for both patients and healthcare professionals, ensuring you’re confident in your health decisions.
Understanding Cardiologist Referral for Borderline ECGs
A borderline ECG can be puzzling. An ECG (electrocardiogram) records your heart’s electrical activity. Sometimes, this recording isn’t clear-cut, showing neither definitive problems nor perfect health. This “gray area” is a borderline ECG. It warrants further investigation, like a check-engine light on a car, suggesting a closer look is needed.
Decoding a Borderline ECG: What Does it Really Mean?
An ECG, a quick and painless test, assesses your heart’s rhythm and electrical signals. Results are typically normal or clearly abnormal. Borderline results, however, fall in between, indicating the need for more investigation but not necessarily a serious heart issue. It is like a blurry snapshot of your heart’s activity; it requires a clearer picture. A borderline ECG suggests subtle deviations from the norm, requiring further evaluation to determine their significance.
Potential Causes Behind a Borderline ECG Result
Various factors can lead to a borderline ECG. Subtle heart rhythm irregularities or less-than-perfectly clear electrical signals during the test are possibilities. Even movement during the test can impact results. Occasionally, a ‘borderline’ reading is just your normal. Your doctor requires more data to pinpoint the cause. Common causes include stress, anxiety, electrolyte imbalances (like potassium or magnesium), certain medications, or even technical errors during the ECG recording. In some cases, borderline ECGs can be the first indication of underlying heart conditions, making further investigation crucial.
Navigating a Borderline ECG: Actionable Steps
While a borderline ECG isn’t cause for panic, it does require action. It’s not an emergency, but it’s a prompt to prioritize your cardiac health. Consulting with your physician is generally the wisest move. Early detection and proactive management are essential for maintaining optimal heart health.
What to Do After a Borderline ECG: A Step-by-Step Approach
- Consult Your Physician: Schedule a discussion regarding your ECG results. Bring a copy of the report and detail any symptoms like chest pain, shortness of breath, dizziness, or a racing heart. Remember to tell your doctor about any medications you are taking, including over-the-counter drugs and supplements. Your doctor’s insight is invaluable. Be prepared to discuss your lifestyle, including diet, exercise habits, and any history of smoking or alcohol consumption.
- Explore Further Testing: Your doctor may advise additional tests for a more detailed view of your heart. Options include:
- Repeat ECG: A second ECG can clarify initial results, especially if the first test was affected by temporary factors like stress or anxiety.
- Stress Test: This monitors heart activity while you exercise, revealing how your heart performs under stress. Different types of stress tests exist, including treadmill tests, bicycle tests, and pharmacological stress tests using medication to simulate exercise.
- Echocardiogram (Echo): Ultrasound creates images of your heart’s structure and function, providing valuable information about valve function, heart muscle strength, and potential abnormalities.
- Holter Monitor: A portable device tracking heart activity over 24+ hours, useful for detecting intermittent rhythm issues that might not be apparent during a brief ECG recording. Event monitors, which record heart activity only when you experience symptoms, may also be considered.
- Consider a Cardiologist Referral: Your doctor might suggest seeing a cardiologist (heart specialist). This doesn’t automatically mean a serious problem; it’s often for expert evaluation and peace of mind. A cardiologist can provide a more in-depth assessment of your heart health and recommend the most appropriate course of action.
- Adhere to Medical Advice: Closely follow your doctor’s recommendations, be it lifestyle adjustments, additional testing, or medication. Transparent communication with your healthcare team is key. Be proactive in asking questions and seeking clarification on any concerns you may have.
Scenarios Warranting a Cardiologist Consultation
While not always necessary, a cardiologist referral is often advised in these cases:
- Concerning ECG Patterns: Suspicious patterns suggesting arrhythmias (irregular heartbeats) or potential structural heart issues exist. Specific ECG abnormalities, such as ST-segment changes or prolonged QTc intervals, may warrant further investigation by a cardiologist.
- Symptom Presence: Symptoms like chest pain, shortness of breath, dizziness, or palpitations accompany the ECG. The presence of these symptoms, especially if they are new or worsening, can indicate an underlying heart condition that requires specialized evaluation.
- Family Medical History: A family history of heart disease or related conditions is present. A strong family history of heart disease significantly increases your own risk, making a cardiologist consultation a prudent step.
- Risk Factors: You have heart disease risk factors like high blood pressure, high cholesterol, diabetes, or smoking. These risk factors, especially when combined, can significantly impact your heart health and warrant monitoring by a cardiologist.
Benefits of Consulting a Heart Specialist
- Specialized Knowledge: Cardiologists excel at ECG interpretation and heart condition diagnosis, offering expert analysis of your results. They have extensive training and experience in identifying subtle ECG patterns that may be missed by general practitioners.
- Comprehensive Evaluation: Thorough exams include detailed medical history reviews, physical assessments, and evaluations of additional tests. Cardiologists take a holistic approach to evaluating your heart health, considering all relevant factors.
- Tailored Treatment: Cardiologists will develop a customized treatment strategy to meet your specific needs and situation after comprehensive evaluations. Treatment plans may include lifestyle modifications, medications, or interventional procedures, depending on the diagnosis.
- Anxiety Reduction: Consulting a cardiologist often eases anxiety, providing specialist insights and reassurance. Understanding your heart health status and having a clear plan of action can significantly reduce stress and improve your overall well-being.
During your appointment, expect discussions about your medical history, a physical exam, a review of test results, and potential treatment options involving lifestyle adjustments, medications, or procedures, depending on findings. The cardiologist will explain your test results in detail and answer any questions you may have.
Remember, a borderline ECG requires investigation, not panic and working in tandem with your healthcare provider to maintain heart health will give you the best results.. Open communication and proactive care are your best allies in maintaining your heart health. Lifestyle modifications, such as adopting a heart-healthy diet, engaging in regular physical activity, and managing stress, can play a crucial role in improving your heart health.
How to Interpret Borderline ECG Results and Next Steps for Proactive Heart Health
A borderline ECG can feel like being in limbo. It requires further exploration to understand the whole picture. Let’s discuss what to do next. Understanding the nuances of borderline ECG results empowers you to take control of your heart health journey.
Decoding Borderline ECGs: Beyond the Surface
A borderline ECG doesn’t automatically indicate a major heart issue. It signals that more information is required. Numerous elements can contribute to a borderline result, spanning from stress to underlying conditions. It’s essential to view a borderline ECG as a prompt for further investigation, rather than a definitive diagnosis.
Decoding the Causes: What Contributes to Borderline ECG Readings?
Many factors can produce a borderline ECG reading, including:
- Stress and Anxiety: Stress-induced heart rate increases affect ECG readings. Elevated levels of stress hormones can disrupt the heart’s electrical activity, leading to borderline results.
- Electrolyte Imbalances: Imbalances in electrolytes like potassium can disrupt heart rhythm. Potassium, calcium, and magnesium play crucial roles in maintaining normal heart function, and imbalances can affect ECG readings.
- Medications: Specific medications might alter ECG results. Certain medications, such as antidepressants, antihistamines, and decongestants, can have an impact on the heart’s electrical activity.
- Technical Issues: Improper electrode placement can sometimes cause artifacts. Ensuring accurate electrode placement is crucial for obtaining reliable ECG recordings.
- Underlying Cardiac Conditions: Rarely, early-stage heart conditions manifest as borderline ECGs. In some cases, a borderline ECG can be the first sign of an underlying heart condition, such as coronary artery disease or arrhythmia.
This is not exhaustive, but it shows the array of impacts on ECG results. Recognizing these potential causes can help guide further investigation and management.
A Step-by-Step Guide: Navigating Borderline ECG Results
- Stay Calm: A borderline ECG is not a diagnosis; it prompts further investigation. It’s important to avoid unnecessary anxiety and focus on gathering more information.
- Engage with Your Physician: Your physician will assess your ECG along with your medical history and lifestyle. Discuss your symptoms, medications, and any relevant family history with your doctor.
- Pursue Further Testing: Your doctor may recommend additional tests, like a repeat ECG, Holter monitor (a portable ECG), or other cardiac evaluations, to get a clearer picture. The specific tests recommended will depend on your individual circumstances and risk factors.
- Consider Lifestyle Adjustments: If appropriate, your physician may suggest stress reduction or dietary changes. Adopting a heart-healthy lifestyle can significantly improve your overall cardiovascular health.
- Maintain Regular Follow-Ups: Schedule regular checkups to track heart health and note any changes. Regular monitoring is essential for detecting any changes in your
- How Much Do Wellness Programs Cost Businesses To Offer? - December 16, 2025
- Wellness Fair Ideas for Work to Boost Employee Wellbeing - December 15, 2025
- Affordable Employee Wellness Fair Ideas for Any Budget - December 14, 2025