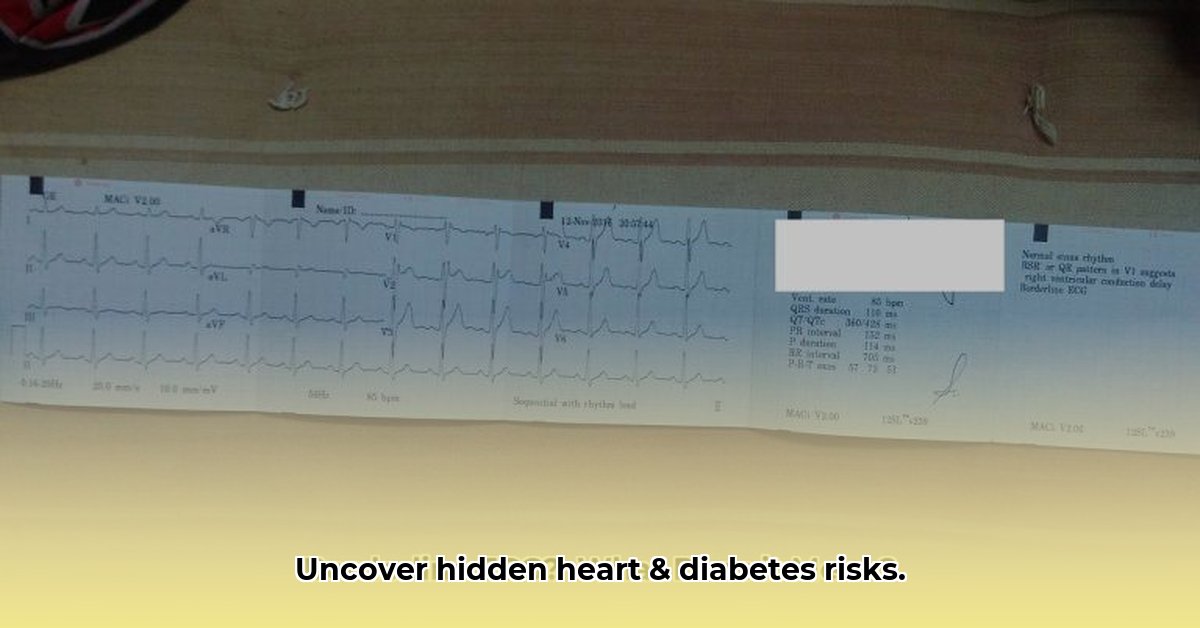
Having diabetes significantly elevates the risk of heart problems, making early detection paramount. Initial warning signs sometimes manifest as subtle anomalies on an electrocardiogram (ECG) – those “borderline” readings that require careful interpretation. This article provides insights into navigating borderline ECGs in the context of diabetes, deciphering common misinterpretations, differentiating between Type 1 and Type 2 diabetes implications, and offering a step-by-step guide to understanding subtle clues. We’ll share expert strategies for improved diabetes management based on ECG results, proactively addressing hidden heart risks and enhancing long-term health.
Borderline ECG and Diabetes: Understanding Your Heart’s Signals for Early Intervention
Diabetes extends beyond blood sugar levels; it significantly heightens the likelihood of heart complications. Early detection is crucial, and electrocardiograms (ECGs) play a vital role in this process. But what does it signify when your ECG results are classified as “borderline”? Let’s explore the importance of ECG in diabetes management and heart health.
Your Heart’s Electrical Blueprint: The ECG
An ECG captures a snapshot of your heart’s electrical activity, illustrating the pathway of electrical signals through your heart, enabling it to beat. In individuals with diabetes, chronic hyperglycemia can damage the blood vessels and nerves supplying the heart. This damage can subtly alter your heart’s rhythm and function, often reflected in ECG readings, serving as an early warning system.
Common ECG changes associated with diabetes encompass an enlarged heart muscle (left ventricular hypertrophy), a delay in electrical recovery (QT prolongation), and irregularities in heart rhythm variations (heart rate variability or HRV). These changes often indicate the insidious damage caused by prolonged high blood sugar levels, increasing the risk of heart problems. Even minor changes to an ECG can increase your risk of a cardiac event.
What “Borderline” Really Means in the Context of Diabetes Management
A “borderline” ECG result in a diabetic individual suggests a deviation from the norm, but isn’t necessarily immediate cause for alarm—it is a yellow light rather than a red one. These findings aren’t dramatically abnormal, but they indicate a heightened risk of future heart issues. For example, a slightly enlarged heart muscle might be acceptable independently, but it suggests your heart might be working harder than it should. Understanding the broader picture of your overall health and diabetes management is essential.
Rather than panic, a borderline ECG signals the need for a more thorough checkup and comprehensive risk assessment.
Interpreting Borderline ECG Results in Diabetes: More Than Just Numbers
Interpreting a borderline ECG in a diabetic individual involves careful assessment of multiple factors:
- Diabetes control: Poorly managed diabetes significantly increases the risk of heart-related complications.
- Existing heart risk factors: High blood pressure, elevated cholesterol, and smoking contribute to increased risk.
- Presence of symptoms: Chest pain, shortness of breath, or irregular heartbeats are crucial indicators.
- Family history: A family history of heart disease increases your inherent risk.
Your healthcare provider considers the overall clinical picture. While a single finding may not be concerning, several factors considered together provide a clearer understanding of your heart’s health.
Next Steps After a Borderline ECG: Taking Control of Your Heart Health
If your ECG reveals borderline changes:
- Consult your doctor: They will assess your case and explain the implications of the results.
- Re-evaluate diabetes management: Improved blood sugar control is the most effective intervention.
- Additional testing: A stress test or echocardiogram might be required.
- Embrace lifestyle changes: A heart-healthy diet, regular exercise, and smoking cessation can significantly improve outcomes.
Addressing the underlying cause—diabetes—is paramount. Stabilizing blood sugar levels reduces stress on your heart.
The Long View: Prevention and Proactive Care for Cardiovascular Wellness
Early detection through ECG monitoring allows for timely intervention. By adopting healthy lifestyle choices and effectively managing diabetes, you can significantly reduce your chances of developing serious heart problems. Regular checkups and open communication with your healthcare team are vital for maintaining heart health. Proactive involvement and early detection can save lives through teamwork between you and your healthcare provider to ensure a strong heart for years to come; in fact, 80% of cardiovascular disease is preventable according to the American Heart Association.
How to Interpret Borderline ECG Findings in Diabetic Patients for Optimal Cardiovascular Outcomes
Key Takeaways:
- Borderline ECGs are inconclusive, requiring further investigation for accurate diagnosis.
- Several factors can cause borderline ECG readings in diabetic patients, necessitating a thorough approach.
- Early detection and prompt action are crucial for improved and sustainable health outcomes.
- AI is improving ECG interpretation, but expert judgment remains essential for nuance.
- Lifestyle modifications play a significant role in managing risk, thereby promoting holistic well-being.
Understanding the Challenge of Borderline ECGs in Diabetes Management
Diabetes significantly increases the risk of cardiovascular disease, highlighting the importance of electrocardiogram (ECGs) in diabetes management. How can you tell the difference between a borderline and normal ECG? A borderline ECG isn’t a definitive diagnosis; it signals the need for further investigation to rule out potential issues. An ECG provides a snapshot of the electrical activity of the heart and helps in identifying abnormalities, which might indicate underlying heart conditions.
What Causes Borderline ECG Findings in Diabetic Patients?
Several factors can contribute to a borderline ECG in diabetic patients:
- Underlying Cardiovascular Disease: Diabetes damages blood vessels, increasing the risk of heart conditions by up to four times.
- Electrolyte Imbalances: Diabetes can affect potassium, calcium, and magnesium levels, impacting the heart’s electrical activity and causing arrhythmia.
- Medication Side Effects: Medications used to treat diabetes or other health issues can alter the ECG rhythm.
- Autonomic Neuropathy: Nerve damage, common in diabetes, can affect heart rate regulation.
- Stress: Stress can trigger changes in heart rhythm and ECG patterns.
- Hyperglycemia-induced Hypoglycemia: Even in healthy individuals, hyperinsulinemia-induced hypoglycemia can prolong the QTc interval and decrease T-wave area and amplitude.
- Genetic Variants: Genetic variants in previously identified candidate genes may be associated with QT interval duration in individuals with diabetes mellitus.
How to Proceed with Borderline ECG Results: Early Intervention Strategies for Better Health Outcomes
Interpreting borderline ECG findings in diabetic patients requires a systematic approach. A borderline ECG isn’t automatically a medical crisis; it calls for further evaluation. Here’s a recommended approach:
- Review Patient History and Symptoms: Assess the patient’s medical history, including existing diabetic complications and symptoms like chest pain, shortness of breath, or palpitations.
- Order Additional Tests: Further investigations might include a stress test, echocardiogram, or Holter monitor, which can give a fuller picture of what is happening.
- Consider Lifestyle Interventions: Encourage lifestyle modifications like healthy eating, regular exercise (aiming for at least 150 minutes of moderate-intensity exercise per week), and stress management techniques.
- Assess Cardiac Autonomic Neuropathy (CAN): Baroreflex dysfunction and disturbed heart rate variability are commonly used methods to assess CAN.
- Evaluate Myocardial Ischemia: Look for painless myocardial ischemia, which is more common in patients with diabetes mellitus. Resting ECG abnormalities, as well as cardiac autonomic dysfunction, can be predictors of silent ischemia in asymptomatic persons with Type 1 Diabetes (T1D).
Risk Assessment and Management Strategies for Long Term Well-being
| Risk Factor | Low Risk | Moderate Risk | High Risk |
|---|---|---|---|
| Age | <50 | 50-65 | >65 |
| Family History of CVD | No history | Family history, but no personal events | Personal history of CVD, or multiple family history cases |
| Diabetes Duration | <5 years | 5-10 years | >10 years |
| Diabetes Type | Well-controlled Type 2 | Type 2 with some complications | Type 1 or poorly controlled Type 2 |
| Diabetic Complications | None | Mild neuropathy or nephropathy | Severe neuropathy, nephropathy, or retinopathy |
| ECG Abnormalities | Minimal deviations | Moderate deviations | Significant deviations |
Note: This table is illustrative. Individual risk profiles should be determined with a medical professional, since 68% of adults with diabetes have hypertension.
The Role of AI in ECG Interpretation: Enhancing Cardiovascular Diagnostic Accuracy
Artificial intelligence (AI) systems assist in ECG interpretation, enhancing—not replacing—the expertise of a cardiologist. AI might reduce the prevalence of borderline readings by increasing detection accuracy. However, AI’s ability to resolve ambiguities remains limited, and these cases need confirmation by a trained professional.
The Importance of QTc Interval
Prolonged QTc Interval. Even in healthy individuals, hyperinsulinemia-induced hypoglycemia can prolong the QTc interval and decrease T-wave area and amplitude. Correlation was found between the QT duration and the amount of coronary calcium; this association was driven by the QRS and not by JT interval duration. Okin et al also found that both QTc prolongation and ST depression predicted all-cause mortality in patients with type 2 diabetes mellitus.
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026
- Essential Meditation Books for Beginners and Experienced Practitioners - January 27, 2026