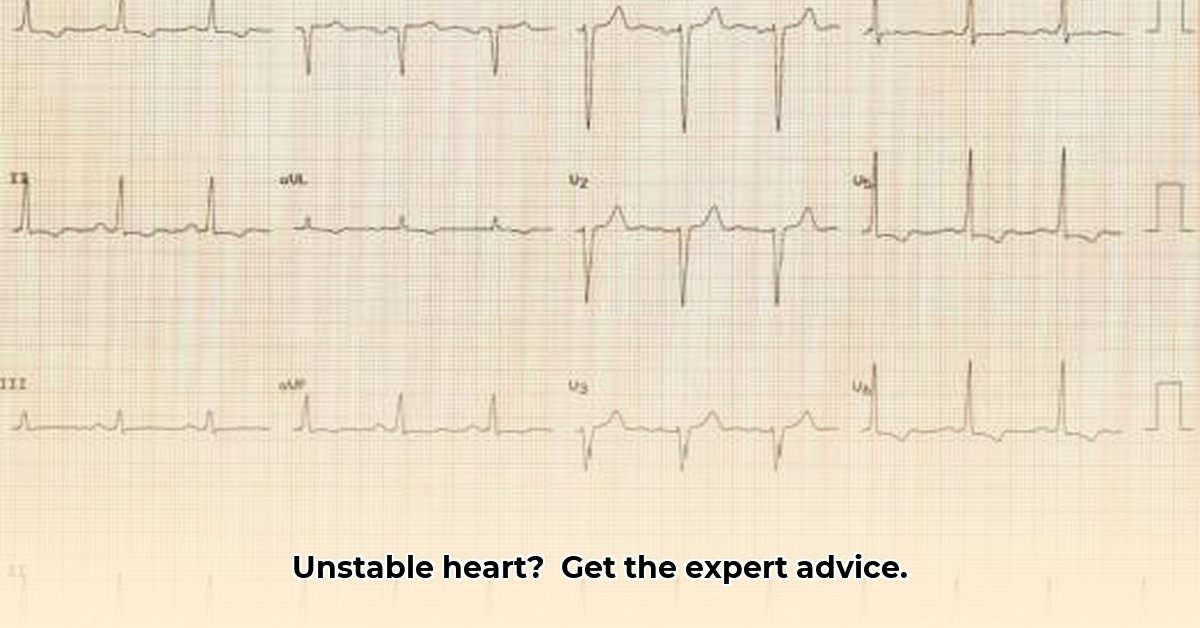
Getting a “borderline” ECG result along with a fast heartbeat can be worrying. This article offers expert advice to help you understand what that means, what might be causing it, and what you should do next, to improve your cardiovascular well-being. For more detailed information on next steps, see this helpful guide: more ECG info.
Borderline ECG and High Heart Rate: Understanding Your Results
A borderline ECG result with a fast heart rate highlights the importance of understanding your heart health. It means your heart’s electrical activity shows some minor quirks on the electrocardiogram (ECG), but nothing definitively wrong. That higher-than-normal heart rate adds a layer of concern.
What Could Be Causing a Borderline ECG and Fast Heartbeat?
Several factors can lead to a borderline ECG and a fast heart rate, affecting heart rhythm and requiring further investigation.
- Temporary Factors: Stress, anxiety, or even dehydration can temporarily mess with your heart rhythm.
- Electrolyte Imbalances: Low potassium, for instance, can show up on your ECG.
- Technical Issues: Improper placement of the ECG electrodes can lead to inaccurate readings.
- Underlying Medical Issues: This could range from a minor heart problem to something more serious, which is why further investigation is crucial.
It’s important to remember that a borderline result doesn’t always mean something significant is wrong. It simply warrants additional examination to rule out any potential problems.
Understanding Your Results: It’s More Than Just Numbers
Interpreting a borderline ECG and a rapid heartbeat isn’t a simple yes or no answer. Your doctor will consider your entire health picture – including your age, medical history, and what symptoms you’re experiencing. The term “borderline” itself isn’t precisely defined; what might be borderline for one person might be totally normal for another.
Next Steps: Working Together to Find Answers
Your healthcare provider is your partner in figuring out what’s going on.
For Patients:
- Follow-Up Appointment: Schedule a visit with your doctor to discuss your results.
- Open Communication: Be clear about all your symptoms. Tell your doctor about anything unusual, like chest pain, dizziness, feeling lightheaded, or shortness of breath.
- Lifestyle Tweaks: Your doctor may suggest simple lifestyle changes, such as managing stress better, getting more regular exercise, and eating a heart-healthy diet.
For Primary Care Physicians (PCPs):
- More Tests, More Information: Your doctor might order more tests to get a clearer picture. These could include another ECG, blood tests (to check for electrolyte imbalances), an echocardiogram (a heart ultrasound), a stress test (to see how your heart works under exertion), or a Holter monitor (which tracks your heart rhythm continuously for 24-48 hours).
- Clear and Compassionate Communication: Your doctor should explain the uncertainty of a borderline ECG and fast heart rate in a way that makes sense.
- Referral to a Specialist (If Needed): If the tests are still inconclusive or if you have worrisome symptoms, your doctor might refer you to a cardiologist for a specialized opinion.
For Cardiologists:
- Expert ECG Review: Cardiologists specialize in interpreting ECGs and will consider your medical history and test results to get a comprehensive understanding.
- Guiding Further Testing: They’ll help decide if any additional tests are needed based on their expert assessment.
- Diagnosis and Treatment Plan: After a thorough evaluation, they’ll provide a diagnosis and a treatment plan to address the underlying cause of your borderline ECG and heart rate.
Lifestyle Matters: Supporting Your Heart Health
Your lifestyle choices play a huge role in your heart health. Regular physical activity, a balanced diet rich in fruits, vegetables, and whole grains, and effective stress management can all positively impact your heart rhythm and ECG results.
When to Seek Immediate Medical Help
While a borderline ECG and a faster-than-normal heart rate aren’t usually emergencies, some symptoms require immediate medical attention. Seek medical help right away if you experience severe chest pain, sudden difficulty breathing, fainting or near-fainting spells, or rapid, irregular heartbeats accompanied by dizziness.
The Bottom Line: It’s a Team Effort
Dealing with a borderline ECG and a high heart rate is a collaborative process. Your healthcare team—your primary care doctor and potentially a cardiologist—will work with you to figure out what’s happening and develop a plan to ensure the best possible care. Remember, many factors can contribute to these results, and further investigation is often the best way to gain clarity and peace of mind. Don’t hesitate to ask your doctor any questions you may have.
How to Interpret Borderline ECG Results and Next Steps
Key Takeaways:
- A borderline ECG isn’t a diagnosis; it flags the need for further investigation.
- Many factors can cause borderline ECG readings, from simple dehydration to serious underlying conditions.
- It involves a collaborative effort between you and your healthcare team.
- Additional tests, lifestyle modifications, and ongoing monitoring are often recommended.
Understanding Borderline ECG Findings
A “borderline” ECG doesn’t mean you have a serious heart problem. Think of it like a traffic light that’s amber—it’s not green (all clear), but not red (stop) either. It signals a need for a closer look. Your doctor uses this ambiguous result to guide the next steps, to determine if further investigation is needed.
Many things can cause this ambiguous reading. Sometimes it’s simply due to minor variations; other times, more in-depth evaluation is warranted. This includes things like temporary changes in electrolytes, dehydration, anxiety, medications, or even a slightly incorrect electrode placement during the test.
What to Do if Your ECG is Borderline
Your next step is a conversation with your doctor. Don’t panic; many people receive borderline ECG results. The result itself isn’t a diagnosis. Your physician will consider several key elements:
- Your Medical History: They will review your past health conditions and any family history of heart problems.
- Your Symptoms: Are you experiencing any chest pains, palpitations, shortness of breath, or dizziness?
- Your Lifestyle: Your diet, exercise habits, stress levels, and any medications you take all play significant parts in interpreting your results.
Based on this information, your doctor will determine the necessity of further testing.
Additional Testing & Next Steps
Here are some possible next steps, depending on your specific case:
- Repeat ECG: Sometimes, a simple repeat ECG can clarify the initial findings.
- Blood Tests: These can reveal electrolyte imbalances.
- Holter Monitor: This portable device tracks your heart rhythm for 24-48 hours, detecting patterns not visible in a standard ECG.
- Echocardiogram: This ultrasound test visually images your heart’s structure and function.
- Stress Test: This assesses your heart’s response to exercise, highlighting potential problems under stress.
Actionable Steps to Take:
- Track Your Symptoms: Keep a detailed record of any symptoms you experience, including when they occur and how long they last. This information can be valuable for your doctor.
- Review Your Medications: Make a comprehensive list of all medications, supplements, and over-the-counter drugs you’re taking, and discuss them with your doctor. Some medications can affect your heart rhythm.
- Adopt a Heart-Healthy Diet: Focus on eating a balanced diet rich in fruits, vegetables, whole grains, and lean protein. Limit processed foods, saturated fats, and sugary drinks. The Mediterranean diet is a good example of a heart-healthy eating plan.
- Incorporate Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week. Find activities you enjoy, such as walking, jogging, swimming, or cycling.
- Manage Stress: Practice stress-reduction techniques like meditation, yoga, deep breathing exercises, or spending time in nature.
- Prioritize Sleep: Aim for 7-8 hours of quality sleep per night.
- Limit Caffeine and Alcohol: Excessive consumption of caffeine and alcohol can sometimes lead to heart rhythm irregularities.
- Quit Smoking: If you smoke, quitting is one of the best things you can do for your heart health.
- Stay Hydrated: Drink plenty of water throughout the day.
- Monitor Your Blood Pressure: Regularly check your blood pressure and work with your doctor to manage it if it’s high.
Understanding Different Types of Heart Rate:
- Resting Heart Rate: This is your heart rate when you’re at rest, such as when you’re sitting or lying down. A normal resting heart rate is typically between 60 and 100 beats per minute.
- Maximum Heart Rate: This is the highest your heart rate should reach during exercise. It’s typically estimated by subtracting your age from 220.
- Target Heart Rate: This is the range of heart rates you should aim for during exercise to get the most benefit. It’s typically between 50% and 85% of your maximum heart rate.
Conditions That Can Cause a High Heart Rate (Tachycardia):
* Atrial Fibrillation (A-Fib): A common
- Top Rated Meditation Books to Deepen Your Practice - February 5, 2026
- Good Mindfulness Books For A Calmer, Happier Everyday Life - February 4, 2026
- Recommended Meditation Books for Beginners and Experienced Practitioners - February 3, 2026