Heart tests (ECGs) are crucial before surgery to check for heart problems. But sometimes, the results are unclear, making it hard for doctors to know what to do. This guide will help surgeons, anesthesiologists, and cardiologists understand those tricky ECGs. We’ll break down how to read them, point out common mistakes, and show you the best ways to handle uncertain results, so you can make the right decisions for your patients and keep them safe.
Borderline ECG in Preoperative Evaluation: A Practical Guide
Interpreting an electrocardiogram (ECG) before surgery can be tricky. Lots of ECGs show minor irregularities, leaving doctors wondering if they’re a big deal or not. This guide helps you understand and manage these borderline cases. We’ll focus on making smart decisions, avoiding unnecessary tests, and keeping patients safe. For more detailed information, see this helpful guide on borderline ECGs.
Understanding Borderline ECG Findings: Seeing Beyond the Lines
Pre-surgery ECGs are common, but they’re not always easy to read. Many show tiny abnormalities that can leave doctors scratching their heads. This isn’t about finding immediate dangers; it’s about carefully considering the whole picture to make the best decisions for your patient. The key is to understand that a borderline ECG is just one piece of the overall patient picture, not the whole story. Are you considering all contributing factors when assessing borderline ECGs?
Deciphering the Heart’s Signals: The Bigger Clinical Picture
You can’t just look at the ECG in isolation. Think of it like a puzzle piece – you need the whole picture. Consider the patient’s age; their past health problems; if they’re currently experiencing any symptoms like chest pains or shortness of breath; and the type of surgery planned. A tiny abnormality might mean nothing for a young, healthy person getting a simple procedure, but could be very important for an elderly person with heart problems facing a major operation.
Interpreting Common Tricky ECG Findings: Decoding the Heart’s Messages
Several ECG patterns often cause confusion. Let’s break down some common ones:
- Mysterious ST-T Wave Changes: These wobbly lines can be caused by lots of things – low oxygen to the heart (ischemia), mineral imbalances (electrolyte abnormalities), medications, or just normal variations in the ECG. The meaning really depends on the patient’s overall health and symptoms. Specific medications like digoxin or antiarrhythmics can significantly alter ST-T waves. Furthermore, conditions such as pericarditis can also manifest with ST-T wave changes.
- Left Ventricular Hypertrophy (LVH): LVH means the heart’s left pumping chamber is thicker than usual. While this can signal increased heart risk, the actual risk depends on other things such as the patient’s symptoms and their ability to exercise (functional capacity). Common causes of LVH include hypertension and aortic stenosis. The Cornell product or the Sokolow-Lyon index are commonly used criteria in ECG interpretation to determine the presence of LVH.
- Left Anterior Fascicular Block (LAFB) and Right Bundle Branch Block (RBBB): These are problems with the heart’s electrical system that can happen even if the heart is perfectly healthy. Having both at once might suggest a higher chance of a heart problem, though. RBBB can be seen in healthy individuals, but it can also be associated with pulmonary embolism or right ventricular hypertrophy. LAFB, on the other hand, is less common in healthy individuals and can be associated with conditions affecting the left ventricle.
- Previous Heart Attack (Myocardial Infarction): Just because someone had a heart attack doesn’t mean they can’t have surgery. However, it does mean a more thorough examination is needed to assess their current risk. It’s about evaluating their current heart health, not just their history. ECG findings indicative of a prior MI include Q waves and ST-segment abnormalities. Cardiac imaging techniques such as echocardiography or cardiac MRI can further assess the extent of myocardial damage.
A Practical Guide: Decoding Borderline ECGs Step-by-Step
Here’s a practical approach:
- The Patient’s Story: Start by carefully reviewing the patient’s medical history, including previous heart problems and current symptoms, any medications they’re taking, and how well they can do physically (their functional capacity). This is crucial for context. Documenting the New York Heart Association (NYHA) functional class can provide valuable insight into the patient’s exercise tolerance.
- ECG Detective Work: Examine the ECG thoroughly, double-checking lead placement (where the electrodes are placed) and looking closely at the heart’s rhythm, intervals between beats, and those ST-T waves. Don’t just rely on the computer’s interpretation – use your judgment. Assess the PR interval, QRS duration, and QT interval. The presence of axis deviation should also be noted.
- Spotting the Imposters (Artifacts): Look carefully for things that might look like heart problems but aren’t – like muscle tremors, incorrectly placed electrodes, or breathing patterns affecting the reading. A repeat ECG often helps clear up these issues. A high-frequency filter can help reduce muscle tremor artifacts.
- Risk Assessment: Use the ECG results, along with other risk factors, to assess how likely the patient is to experience a heart problem during or after surgery. There are special tools and scores to help with this (like the Revised Cardiac Risk Index). The American College of Cardiology/American Heart Association (ACC/AHA) guidelines provide recommendations for preoperative cardiac risk assessment.
- Teamwork Makes the Dream Work: Discuss your findings with the surgeon and anesthesiologist. Combine your knowledge to reach a shared plan. This needs everyone’s input. A multidisciplinary approach involving shared decision-making is essential for optimal patient care.
- When to Call in the Experts: If needed, refer the patient to a heart specialist (cardiologist) for more in-depth evaluation, such as stress testing or advanced imaging. Sometimes an expert opinion is essential for peace of mind. Stress echocardiography and myocardial perfusion imaging are non-invasive techniques that can assess for myocardial ischemia.
Seeking Expert Guidance: Knowing Your Limits
Here’s when you might want to ask for a specialist’s help:
- Major Surgery: Even small ECG changes can be important before risky operations. It’s safer to get a second look. High-risk surgeries such as aortic or major vascular surgery warrant careful consideration of any ECG abnormalities.
- Symptomatic Patients: If the patient is experiencing symptoms like chest pain or shortness of breath, a more thorough heart check is crucial. Symptoms suggestive of cardiac ischemia should prompt further investigation.
- Unclear Findings: If the ECG is still confusing after you’ve looked at it carefully, it’s best to get another doctor’s opinion or do some more tests. An electrophysiology study may be required to evaluate complex arrhythmias.
- Other Health Issues: If the patient has other health problems, it’s even more important to be very careful with their heart evaluation. Patients with diabetes, renal insufficiency, or a history of heart failure require a comprehensive cardiac assessment.
The Importance of Collaboration: It’s a Team Effort
Handling borderline ECGs isn’t about strict rules. It’s about careful thought and collaboration. Combine the ECG with the patient’s whole health story. Work with your colleagues. This thoughtful approach helps ensure you’re making smart decisions, avoiding unnecessary tests, and most importantly, keeping your patients safe. Remember, ongoing research constantly refines our understanding of ECG interpretation and risk assessment; always stay up-to-date with current best practices. Familiarize yourself with the latest guidelines and recommendations from professional societies such as the ACC/AHA and the European Society of Cardiology (ESC).
Differentiating ECG Pathology from Artifact: True Preoperative Cardiac Assessment
Key Takeaways:
- Routine preoperative ECGs are often unnecessary for asymptomatic, low-risk patients. The “Choosing Wisely” campaign recommends against routine ECG screening in this population.
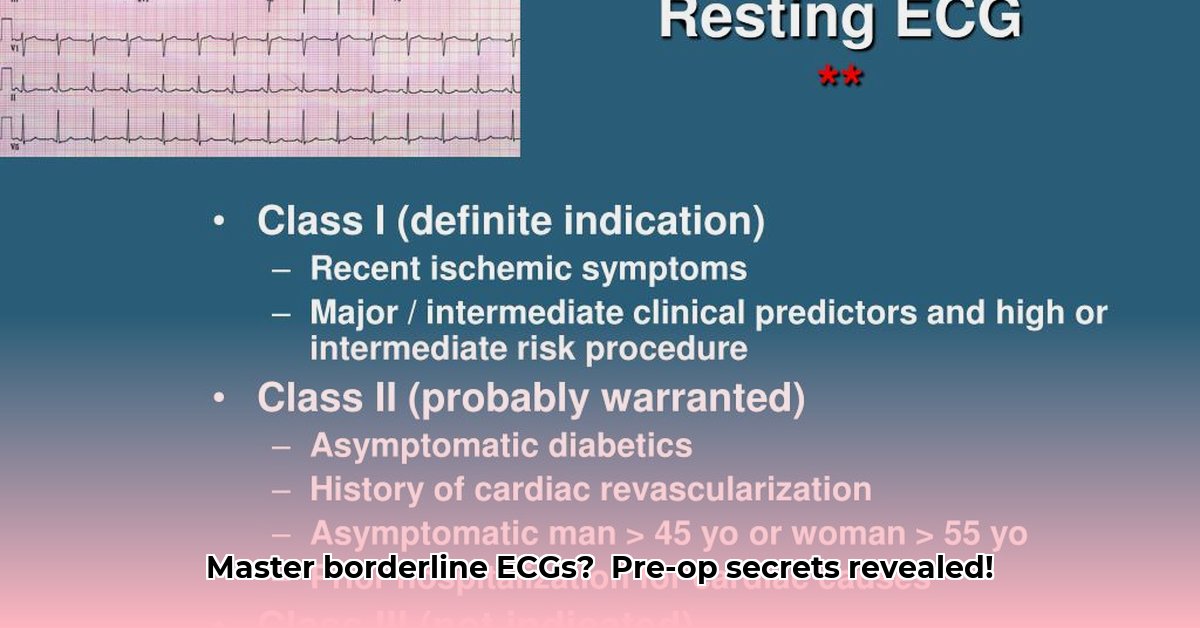
- The ECG’s primary value lies in identifying significant abnormalities in symptomatic patients or those undergoing high-risk procedures. Preoperative ECG is reasonable for patients with known coronary heart disease, significant arrhythmia, peripheral arterial disease, cerebrovascular disease, or significant structural heart disease.
- Careful interpretation is crucial, distinguishing true cardiac pathology from artifacts and normal variations. Proper lead placement and awareness of respiratory variations are essential for accurate ECG interpretation.
Preoperative ECG interpretation presents a unique challenge: how to differentiate true ECG pathology from artifact in order to make informed decisions about surgical risk. It’s a balancing act. We need to identify genuine cardiac issues that might threaten a patient during or after surgery but also must avoid unnecessary delays or interventions caused by misinterpreting harmless variations or technical glitches. The ECG’s interpretation relies heavily on context.
Identifying ECG Artifacts: Recognizing False Signals
Artifacts are essentially “noise” on the ECG tracing. They’re not reflections of the heart’s electrical activity. Common culprits include:
- Wandering baseline: This looks like a slow drift up or down. Muscle movement is usually the cause. Inadequate skin preparation or loose electrodes can contribute to wandering baseline.
- 60-cycle interference: This shows up as rhythmic, repeating artifacts—caused by electrical interference from nearby equipment. Ensure that ECG equipment is properly grounded and that there are no nearby sources of electrical interference.
- Somatic tremor: This manifests as irregular, high-frequency waves, often due to patient
- Top Rated Meditation Books to Deepen Your Practice - February 5, 2026
- Good Mindfulness Books For A Calmer, Happier Everyday Life - February 4, 2026
- Recommended Meditation Books for Beginners and Experienced Practitioners - February 3, 2026