Got a slightly unclear result from your recent heart checkup? A “borderline” ECG (electrocardiogram) can cause concern, but remember it doesn’t automatically signify a serious problem. It simply indicates your doctor requires more details. This article clarifies what a borderline ECG entails, possible causes, and recommended actions. We’ll explain everything plainly, easing your understanding and worries. For more in-depth information, see this helpful guide on borderline ECGs.
Deciphering Borderline ECG Results for Peace of Mind
Receiving a “borderline” ECG result during a routine checkup is understandable if it leaves you puzzled or anxious. Let’s demystify it and provide some clarity about heart health.
What Does “Borderline ECG” Actually Mean for Your Heart Health?
A borderline ECG result during a routine checkup doesn’t automatically indicate a serious heart ailment. Think of it as your heart’s electrical activity—as seen on the ECG—appearing somewhat ambiguous rather than a definitive normal or abnormal reading. Due to this ambiguity, more investigation is required. It suggests a need for a closer examination to ensure accurate cardiac assessment. The term “borderline” suggests the results fall into a gray area, necessitating further scrutiny.
Why Might Your ECG Show Borderline Readings? Exploring Potential Causes
Several factors can contribute to a borderline ECG reading, and it’s not always cause for alarm. Understanding these potential factors can help alleviate unnecessary stress. Here are some potential explanations for heart rhythm variations:
- Stress and Anxiety: Stress influences your body, including your heart. Stress hormones impact your heart rate and rhythm, potentially causing irregular readings. Recent stressful events, such as work deadlines or family problems, can manifest on an ECG. Managing stress through techniques like meditation or deep breathing can positively influence future ECG results.
- Electrolyte Imbalances: Your body requires a balance of electrolytes like potassium, sodium, calcium, and magnesium for proper heart function. Imbalances could reflect in your ECG, but are typically easily corrected through dietary adjustments or, in some cases, medical intervention.
- Medications: Certain prescription and over-the-counter medications, including some cold remedies and herbal supplements, can temporarily affect your heart rhythm, which is normal and doesn’t necessarily signal a heart issue. Always inform your doctor about all medications you are taking for an accurate assessment.
- Technical Glitches: Sometimes, technique matters. Improper electrode placement, faulty equipment calibration, or even slight patient movement during the test can yield inaccurate results. A repeat test could resolve this concern. Ensuring proper technique is crucial for accurate ECG readings.
- Lifestyle Factors: Caffeine, alcohol, smoking, recreational drugs, and intense physical activity can temporarily influence your heart rate and rhythm. Recent consumption or activity might impact results, but these effects are often temporary and usually don’t indicate underlying cardiac conditions.
- Age-Related Changes: As we age, the heart’s electrical pathways can undergo subtle changes, leading to borderline ECG results. These changes don’t always indicate a serious problem but warrant careful monitoring.
Even healthy individuals, including athletes, can occasionally exhibit borderline ECGs. Athletes heart rhythms often differ slightly due to their training regimen, a phenomenon known as “athlete’s heart.” These variations are usually benign but should still be evaluated by a physician.
Your Action Plan: Next Steps After a Borderline ECG
A borderline ECG prompts taking subsequent measures, emphasizing calmness and proactivity. It requires follow-up and a consultation with your doctor. Expect a conversation with your physician and possibly additional tests.
Step 1: Consult Your Doctor: Schedule an appointment to discuss your results. Inform your doctor about any symptoms, even minor ones, such as palpitations, lightheadedness, or fatigue. Your medical history matters, so ensure you present a comprehensive overview, including any family history of heart disease.
Step 2: Further Evaluation and Diagnostic Testing: Your doctor may recommend further tests for clarity. Common follow-up tests include:
- Stress Test: Monitors heart rhythm and function during exercise (or simulated exercise via medication) to assess heart response to stress. This helps identify potential blockages or abnormalities that may not be apparent at rest.
- Echocardiogram: An ultrasound visualizing your heart’s structure, valves, and pumping efficiency. This provides detailed information about the heart’s anatomy and function.
- Holter Monitor: A portable device worn for 24-48 hours, continuously recording your heart’s electrical activity for a comprehensive rhythm assessment. This captures any intermittent arrhythmias that may not be detected during a brief ECG.
- Event Monitor: Similar to a Holter monitor, but worn for a longer period (up to 30 days) and activated by the patient when they experience symptoms.
- Blood Tests: Checks for electrolyte imbalances, thyroid abnormalities, and other factors that may be affecting your heart rhythm.
- Cardiac CT Scan or MRI: In some cases, your doctor may recommend these advanced imaging techniques to get a more detailed view of your heart.
Step 3: Lifestyle Adjustments: Based on overall health and test outcomes, your doctor might suggest lifestyle changes, such as regular exercise, a healthier diet, stress reduction, smoking cessation, or limiting caffeine and alcohol, supporting cardiovascular health. Even small changes can make a significant difference.
When Is Immediate Medical Attention Needed?
While a borderline ECG is usually not urgent, seek prompt medical care if you experience the following:
- Chest Pain: Any chest pain, pressure, or discomfort, especially if it’s new, severe, or radiating to the arm, jaw, or back, necessitates immediate evaluation.
- Shortness of Breath: Sudden or worsening breathing difficulty requires urgent medical attention.
- Dizziness or Fainting: Episodes of fainting or dizziness, particularly if accompanied by chest pain or palpitations, might indicate urgent medical concerns.
- Irregular Heartbeat: A noticeably irregular or rapid heartbeat, especially if it’s sustained or causing discomfort, requires immediate medical advice.
- Sudden Weakness or Numbness: Especially if on one side of the body, may indicate a stroke and requires immediate medical attention.
Bringing It All Together: Moving Forward With Confidence
A borderline ECG often prompts further investigation, but it’s not a diagnosis of a serious condition. Doctors use a cautious approach to ensure patient wellbeing. By following up with your doctor and undergoing recommended tests, you’ll gain insight into your heart health and address potential issues. Remember to openly communicate any concerns or questions you may have.
Summary Table: Potential Causes and Actions
| Potential Cause | Likely Next Steps |
|---|---|
| Stress & Anxiety | Repeat ECG after stress reduction, stress management techniques, consider counseling or therapy |
| Electrolyte Imbalances | Blood tests, dietary adjustments, consider consulting a registered dietitian |
| Medications | Medication review, potential adjustments with your doctor, explore alternative medications if appropriate |
| Technical Issues | Repeat ECG with improved technique, ensure proper electrode placement and equipment calibration |
| Lifestyle Factors | Lifestyle modifications, such as dietary changes, regular exercise, smoking cessation, and limiting alcohol and caffeine intake |
| Age-Related Changes | Regular monitoring, lifestyle modifications, further testing as needed |
| Possible Heart Condition | Echocardiogram, stress test, Holter monitor, event monitor, blood tests, cardiac CT or MRI |
Don’t hesitate to ask your doctor questions about your borderline ECG results and the recommended next steps. Your active participation in your health care is essential for optimal outcomes.
Interpreting Borderline ECG Results: Step-by-Step Guide
A borderline ECG result can be unsettling, indicating that your electrocardiogram (measuring heart’s electrical activity) showed readings that weren’t clearly normal or abnormal. This isn’t automatically a sign of serious heart problems. It warrants further investigation.
Understanding a Borderline ECG
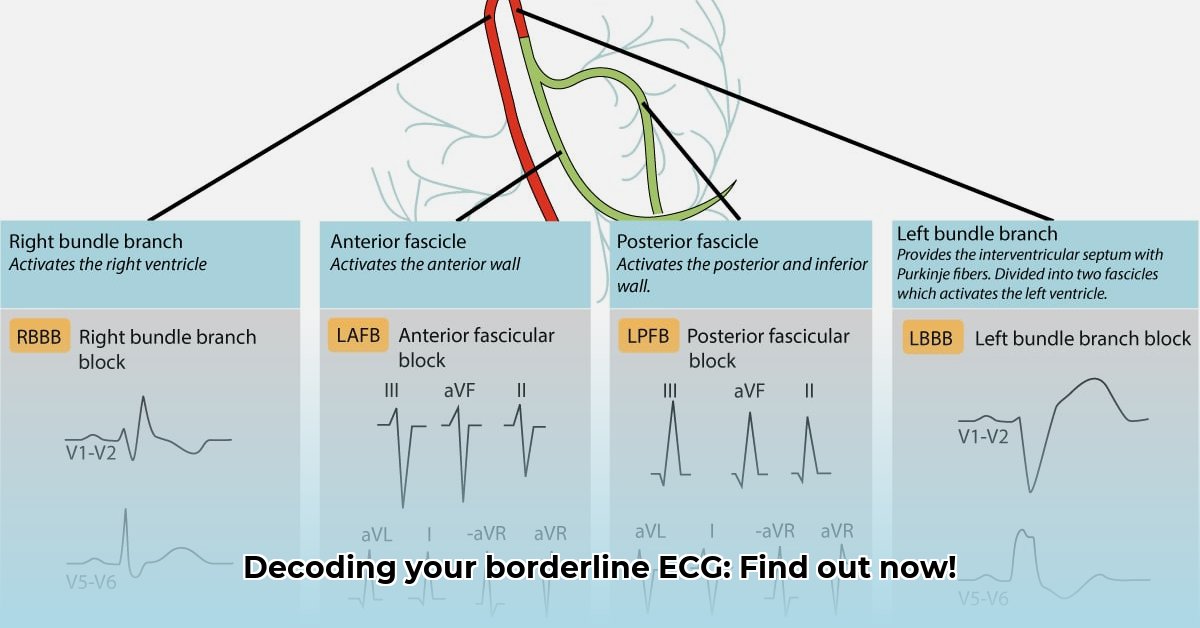
A borderline ECG often signifies minor rhythm or electrical signal variations. These variations can stem from stress, dehydration, caffeine, or certain medications. Technical issues during the test can also alter results. Importantly, a borderline ECG isn’t a diagnosis but necessitates further evaluation to rule out any underlying cardiac issues.
How to Interpret Borderline ECG Results: A Step-by-Step Guide to Heart Health
Understanding how to interpret borderline ecg results and next steps requires a collaborative approach with your doctor, considering your individual circumstances. Here’s what to do:
- Discuss with Your Doctor: Schedule an appointment to discuss your results, allowing your physician to review the ECG specifics and correlate them with your medical history and symptoms. Be prepared to provide a detailed account of any symptoms you’ve been experiencing.
- Seek a Second Opinion: A second opinion from another cardiologist may offer additional perspective, especially if the findings remain ambiguous, leading to a more comprehensive understanding of your heart health .
- Repeat the ECG: Repeating the ECG is often the initial step in this process, aimed at eliminating potential errors from the initial assessment. This helps ensure the accuracy of the results.
- Additional Tests and Cardiac Monitoring: Depending on risk factors, age, and symptoms, your doctor might recommend further tests, including a Holter monitor (a portable ECG tracking heart rhythm over 24-48 hours), an event monitor, an echocardiogram, or a stress test. These tests provide more detailed information about your heart’s function and rhythm over time.
- Lifestyle Modifications for Long-Term Health: Lifestyle changes are beneficial regardless of
- Wellness Fair Ideas for Work to Boost Employee Wellbeing - December 15, 2025
- Affordable Employee Wellness Fair Ideas for Any Budget - December 14, 2025
- Employee Wellness Programs Strategically Benefit Employee Health And Retention - December 13, 2025