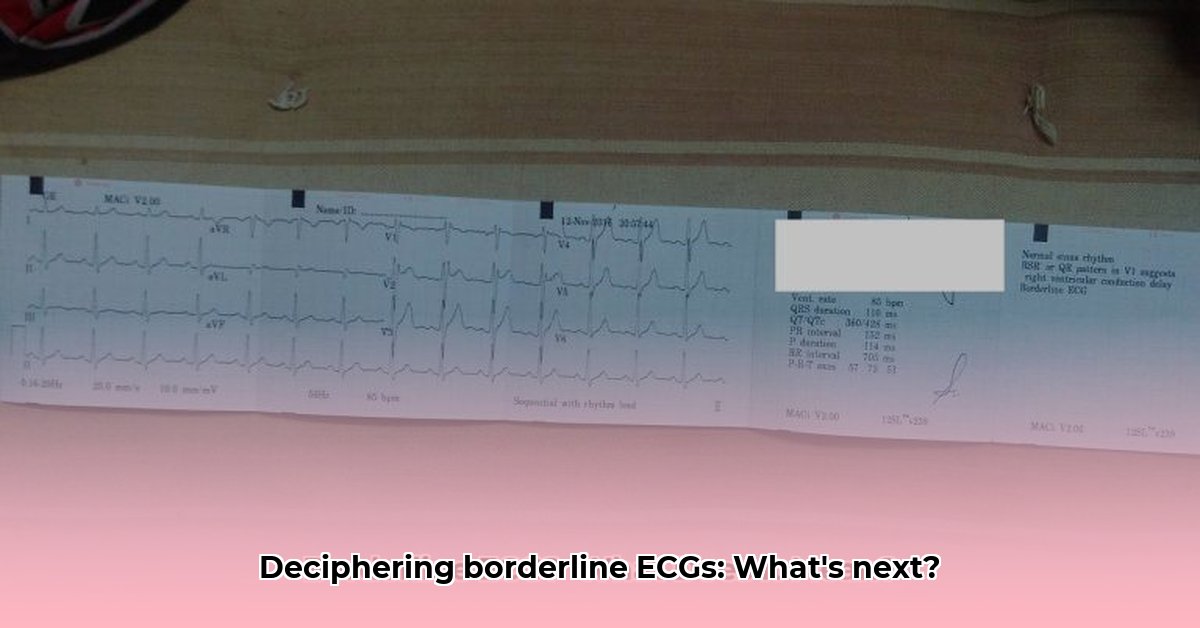
Getting a “borderline” result on your electrocardiogram (ECG) – that heart tracing test – can be worrying. This article aims to take the mystery out of what that means. We’ll explain what causes borderline ECGs, how doctors interpret them, and what you should do next. It’s written for everyone wanting to understand their results and healthcare professionals wanting a clearer picture. Our goal is to give you the information you need to feel confident and informed about your heart health.
Decoding Borderline ECG Medical Terminology
Getting a “borderline” ECG result can feel a bit like walking into a fog. Your heart’s electrical activity shows some slight quirks, nothing alarming on its own, but not quite normal either. It’s not a clear-cut diagnosis, more of a “let’s investigate further” situation. Think of your heart as a finely tuned engine. A borderline ECG suggests a few minor misfires, but we don’t know if it’s a temporary hiccup or something that needs attention. What underlying issues might trigger these subtle electrical changes in the heart? This isn’t necessarily a cause for alarm, but it does need a closer look.
This article aims to shed light on what a borderline ECG means and what you can expect next. We’ll explore possible causes, explain the next steps your doctor might take, and offer tips on managing any anxieties you might have. Remember, we’re talking about probabilities, not certainties. Medical science is always evolving, and new research might change our understanding of these subtle findings over time.
What Might Cause a Borderline ECG Result? Potential Heart Rhythm Changes
Several factors can lead to a borderline ECG reading. Let’s explore some common possibilities:
- Electrolyte Imbalances: Your body’s levels of potassium, magnesium, and calcium play a crucial role in your heart’s rhythm. Even slight imbalances can show up on an ECG. These imbalances are often easily correctable through dietary adjustments or, in some cases, supplementation guided by your physician.
- Stress and Anxiety: Believe it or not, feeling stressed or anxious can temporarily throw off your heart rhythm. Your heart rate increases, and the electrical signals might become irregular. This is often temporary and resolves once the stress subsides. Chronic stress, however, can have a more lasting impact on heart health.
- Minor Heart Rhythm Variations: Sometimes, your heart naturally produces extra beats or has slight variations in its rhythm – these are often perfectly normal! Conditions like sinus arrhythmia, where your heart rate changes slightly with your breathing, are quite common, especially in young, healthy individuals.
- Medication Side Effects: Many medications, both prescription and over-the-counter, can affect your heart rhythm as a side effect. This is something your doctor will consider when reviewing your current medications. Common culprits include decongestants, certain antidepressants, and some herbal supplements.
- Technical Glitches: Occasionally, a borderline result is simply due to a technical issue during the ECG procedure. This could be something as simple as an incorrectly placed electrode, resulting in a slightly distorted reading. A repeat ECG, performed with careful attention to detail, often clarifies this.
- Underlying Medical Conditions: In some cases, a borderline ECG might hint at an underlying heart condition or other health issues that need further investigation. This is why additional tests are important. Conditions such as high blood pressure, thyroid disorders, and even sleep apnea can impact heart rhythm.
Interpreting Your Borderline ECG: The Next Steps for Assessment
Your doctor will be your guide through this process. They will carefully consider your specific situation, including any symptoms you might be experiencing and your overall health history. Here’s what you can generally expect:
Step 1: The Thorough Review: Your doctor will carefully review your medical history, including any pre-existing conditions, medications you’re taking, and any symptoms you’ve noticed. This helps establish a baseline understanding of your health. Why is a comprehensive medical history so critical in deciphering a borderline ECG? Because it helps differentiate between a potentially serious new finding and a pre-existing condition or medication side effect.
Step 2: The Physical Check-Up: A thorough physical exam will help assess your overall health and look for any physical signs or symptoms that might connect to the ECG findings. This may include checking your blood pressure, listening to your heart and lungs, and looking for any signs of swelling or fluid retention.
Step 3: Further Investigations: Based on the initial review and physical exam, your doctor will determine if additional tests are necessary. These may include:
| Test | Purpose |
|---|---|
| Repeat ECG | To rule out technical errors and see if the abnormality is consistent. |
| Blood Tests | To check your electrolyte levels (potassium, magnesium, calcium) and other markers, as well as thyroid function and kidney function. |
| Stress Test | To see how your heart responds to exercise, helping to detect any underlying coronary artery disease or arrhythmias. |
| Echocardiogram (ultrasound) | To create a detailed picture of your heart’s structure and function, including the heart valves and chambers. |
| Holter Monitor (24-48 hours) | A portable ECG worn for an extended period to monitor your heart rhythm throughout the day, capturing any intermittent abnormalities. |
| Event Monitor | Similar to a Holter monitor, but worn for a longer period (up to 30 days) and activated only when you experience symptoms. |
Living with a Borderline ECG: Your Role in Heart Health Improvement
A borderline ECG is not necessarily a sign of a serious heart problem. Many individuals receive this result and experience no further cardiac issues. However, working closely with your doctor to understand and address potential causes is crucial. What kind of lifestyle adjustments can dramatically impact heart health? Lifestyle adjustments such as adopting a heart-healthy diet, engaging in regular physical activity, maintaining a healthy weight, managing stress, and quitting smoking can significantly improve cardiovascular health.
Lifestyle Adjustments: While the results don’t automatically imply you need major changes, certain lifestyle adjustments can always improve your overall wellness. This could include:
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week. Find activities you enjoy, such as brisk walking, swimming, cycling, or dancing.
- Stress Management: Explore stress-reduction techniques like yoga, meditation, or deep breathing exercises. Consider mindfulness practices or spending time in nature.
- Healthy Eating: Follow a balanced diet rich in fruits, vegetables, and whole grains. Limit processed foods, sugary drinks, and unhealthy fats. The DASH (Dietary Approaches to Stop Hypertension) diet is often recommended for heart health.
- Symptom Monitoring: Pay attention to any changes in your heart rate, chest pain, shortness of breath, or dizziness, and report them to your doctor immediately. Keep a log of your symptoms, including when they occur and what you were doing at the time.
Open Communication is Key: Don’t hesitate to ask your doctor any questions you have. Express your concerns openly and work collaboratively to understand the next steps and make informed decisions about your health. A proactive approach, combined with your doctor’s expertise, will help you manage your heart health effectively. Remember, ongoing research continually shapes our understanding of heart rhythms. Let your doctor keep you informed of any new developments relevant to your specific case. Discuss any new symptoms or concerns you have with your doctor promptly.
How to Interpret Borderline ECG Results and Next Steps
Key Takeaways:
- A borderline ECG isn’t a diagnosis; it’s a signal for further investigation.
- Many factors—from technical glitches to underlying health issues—can cause borderline results.
- Your doctor will consider your medical history, symptoms, and the ECG itself to determine next steps.
- Further testing might include repeat ECGs, echocardiograms, or stress tests.
- A healthy lifestyle plays a significant role in heart health, regardless of ECG results.
Understanding Borderline ECG Findings For Accurate Diagnosis
So, you’ve received a borderline ECG result. What does that mean? It simply means your electrocardiogram shows some slight deviations from what’s considered perfectly normal, but not enough to be definitively diagnosed as abnormal. Think of it like this: it’s a yellow traffic light – caution is advised, but it doesn’t automatically mean you need to stop. The ambiguity is the challenge. It requires further investigation to determine if there’s a reason for concern or if it’s a minor variation. On average, what percentage of borderline ECG findings eventually lead to a significant cardiac diagnosis? It’s difficult to provide a precise percentage, as it varies depending on the population studied and the specific criteria used to define “significant cardiac diagnosis.” However, studies suggest that a significant proportion of individuals with borderline ECGs do not develop serious heart problems.
Often, these borderline findings are due to harmless factors. Stress, dehydration, or even the way the electrodes were placed can slightly alter the readings. Electrolyte imbalances also play a part. Sometimes, however, it could signal the early stages of a heart problem. This is why a doctor’s assessment is crucial. The skill and experience of the interpreting physician are critical in differentiating harmless variations from potentially significant abnormalities.
How to Interpret Borderline ECG Results and Next Steps: A Doctor’s Perspective on Potential Risks
Your physician will carefully review your ECG alongside your medical history. This includes family history of heart conditions and any symptoms you’ve experienced—chest pain, palpitations, shortness
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026