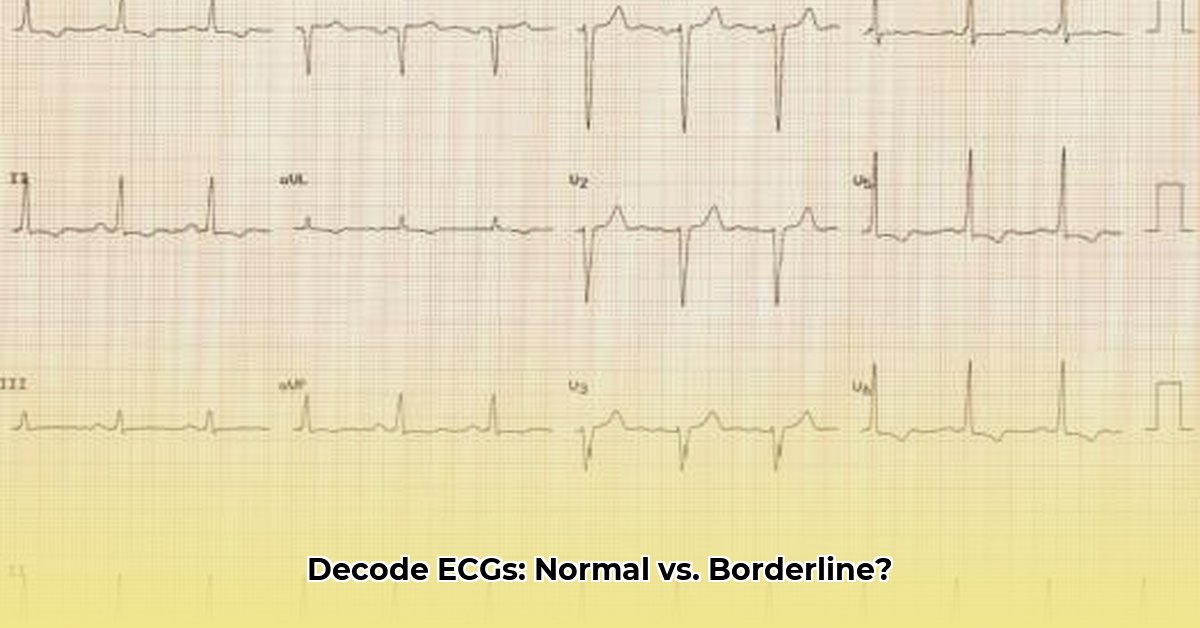
Worried about your ECG results? Seeing the word “borderline” and not sure what it means? This guide will help you understand the difference between a normal and a borderline ECG. We’ll explain what a borderline ECG is, what might cause it, and what you should do next for proactive health management. It’s all about understanding your heart health better and knowing what questions to ask your doctor. For more in-depth information on next steps, see this helpful guide: Next Steps After a Borderline ECG.
Borderline ECG vs Normal: A Comprehensive Guide
Understanding your electrocardiogram (ECG) results can feel like deciphering a complex code, especially when assessing cardiovascular health. While a normal ECG shows your heart working smoothly, a borderline ECG presents a more nuanced picture, requiring careful interpretation. This guide will help you understand the differences and what to do if your ECG comes back with borderline results, empowering you with knowledge for informed decision-making.
Defining a Normal ECG
Imagine your heart as a finely tuned engine, rhythmically pumping blood throughout your body. An ECG is a recording of the electrical signals that control this vital process. A normal ECG demonstrates a steady, consistent rhythm, indicating that your heart’s electrical system is functioning correctly. It signifies a healthy, harmonious flow. The key characteristics include a regular heartbeat, a consistent heart rate within the normal range for your age and activity level, and clear, predictable electrical complexes (P wave, QRS complex, and T wave) in the expected sequence and morphology. Let’s explore these components in more detail, ensuring clarity about heart function:
- P Wave: Represents atrial depolarization, the electrical activity that causes the atria (upper chambers of the heart) to contract. A normal P wave indicates that the atria are functioning correctly.
- QRS Complex: Represents ventricular depolarization, the electrical activity that causes the ventricles (lower chambers of the heart) to contract. The shape, duration, and amplitude of the QRS complex should fall within specific ranges to be considered normal.
- T Wave: Represents ventricular repolarization, the electrical activity that occurs as the ventricles relax and prepare for the next contraction. A normal T wave has a specific shape and direction.
- PR Interval: This measures the time it takes for the electrical impulse to travel from the atria to the ventricles. A normal PR interval ensures proper coordination between atrial and ventricular contractions.
- QT Interval: This measures the total time it takes for the ventricles to depolarize and repolarize. A prolonged QT interval can indicate an increased risk of certain arrhythmias.
Decoding the Borderline ECG: Nuances and Implications
A borderline ECG doesn’t automatically signal a serious heart problem. Instead, it indicates minor deviations from a perfectly normal rhythm or electrical signal patterns. These subtle variations might include small inconsistencies in the heartbeat’s regularity, slight abnormalities in the electrical wave shapes or intervals, or minor variations in the heart rate. Think of it as a slightly off-key note in an otherwise beautiful symphony—not necessarily catastrophic, but definitely worth investigating. It’s a signal to thoroughly investigate further, not a reason to panic, promoting a proactive and informed approach to your health.
Comparing Normal vs. Borderline ECGs: A Detailed Chart
Let’s directly compare a typical ECG result to one showing borderline findings. It’s crucial to consider the context of your overall health; your doctor considers more than just the ECG. They take into account your complete medical history, current symptoms, and lifestyle factors, all vital for accurate diagnostics:
| Feature | Normal ECG | Borderline ECG |
|---|---|---|
| Heart Rhythm | Steady, consistent beat like a metronome | Slightly irregular; maybe a few premature atrial contractions (PACs) or premature ventricular contractions (PVCs), or slight pauses here and there |
| Heart Rate | Within the healthy range (typically 60-100 beats per minute) for your age and activity level | Slightly faster (tachycardia) or slower (bradycardia) than usual, but not alarmingly so. The rate may fluctuate more than expected with respiration or activity. |
| P Wave | Present, consistent shape, and precedes each QRS complex | May be slightly altered in shape or amplitude. In some cases, may be absent or difficult to identify. |
| PR Interval | Consistent duration, typically between 0.12 and 0.20 seconds | May be slightly prolonged or shortened, indicating a potential issue with AV node conduction. |
| QRS Complex | Narrow, consistent shape, typically less than 0.12 seconds in duration | May be slightly widened or have subtle changes in morphology, potentially indicating a conduction delay or ventricular hypertrophy. |
| ST Segment | At baseline, neither elevated nor depressed | Minor, non-specific ST-segment elevation or depression. These changes are often subtle and may not be indicative of acute ischemia. |
| T Wave | Upright and symmetrical in most leads | May be inverted, flattened, or peaked in certain leads. These changes can be non-specific but may suggest ischemia, electrolyte imbalances, or other cardiac abnormalities. |
| QT Interval | Duration appropriate for the heart rate (corrected QT interval, or QTc, is often used) | May be slightly prolonged, increasing the risk of torsades de pointes, a life-threatening arrhythmia. |
| Other Findings | No other significant abnormalities detected | May have a hint of an irregular rhythm, evidence of old myocardial infarction (MI), or other subtle abnormalities that warrant further investigation. |
Possible Causes of Borderline ECG Results
A borderline ECG result doesn’t automatically indicate a serious heart problem but requires further evaluation to determine the underlying cause. Many factors can contribute to these minor deviations. Some possibilities include:
- Electrolyte Imbalances: Temporary electrolyte imbalances (meaning your body’s levels of minerals like potassium, calcium, or magnesium are slightly off) can affect the heart’s electrical activity.
- Medication Side Effects: Certain medications, such as diuretics, antiarrhythmics, or antidepressants, can influence heart rate, rhythm, and ECG patterns.
- Stress and Anxiety: Recent stress, anxiety, or panic attacks can cause temporary changes in heart rate and rhythm, leading to borderline ECG findings.
- Caffeine or Alcohol Consumption: Excessive intake of caffeine or alcohol can sometimes trigger arrhythmias and affect ECG results.
- Underlying Medical Conditions: Conditions like hyperthyroidism, anemia, or sleep apnea can indirectly affect the heart and lead to borderline ECGs.
- Technical Factors: Improper electrode placement, patient movement during the ECG, or electrical interference can sometimes lead to inaccurate readings.
- Normal Variation: In some cases, borderline ECG findings may represent normal variations in heart physiology, particularly in young, healthy individuals or athletes.
Action Plan: Responding to a Borderline ECG
A borderline ECG isn’t a reason to panic, but it is a signal to seek professional medical advice and take proactive steps. Here’s what you need to do to manage cardiac risk factors and understand what influences heart function:
- Schedule a visit with your doctor: Don’t delay; discuss your ECG results with your physician as soon as possible. They can properly interpret your borderline readings in the context of your overall health and risk factors.
- Prepare clarifying questions: Don’t hesitate to ask your doctor to explain any parts of the report you don’t fully understand. For example:
- What specific borderline findings were observed on the ECG?
- What are the potential causes of these findings in my case?
- What are the possible implications for my heart health?
- What are the next steps you recommend, and why?
- Consider further testing: Your doctor may recommend additional tests to gather more information and rule out any underlying cardiac conditions. These tests might include:
- Blood Tests: To check electrolyte levels, thyroid function, and cardiac enzymes (e.g., troponin).
- Holter Monitor: A 24-hour (or longer) ambulatory ECG monitor to assess your heart rhythm over an extended period.
- Echocardiogram: An ultrasound of your heart to evaluate its structure and function.
- Stress Test: To assess how your heart responds to exercise and identify any signs of ischemia (reduced blood flow to the heart).
- Cardiac CT or MRI: In some cases, these advanced imaging techniques may be used to visualize the heart in more detail.
- Adopt a Heart-Healthy Lifestyle: Regardless of the underlying cause of the borderline ECG, adopting a heart-healthy lifestyle can help improve your overall cardiovascular health. This includes:
- Eating a balanced diet rich in fruits, vegetables, whole grains, and lean protein.
- Engaging in regular physical activity (at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity exercise per week).
- Maintaining a healthy weight.
- Mindfulness Exercises For Anxiety PDF To Reduce Stress - February 26, 2026
- Mindfulness Activities for Adults PDF for Stress Relief - February 25, 2026
- Mindfulness Techniques PDF Offers Free Exercises for Calm and Focus - February 24, 2026