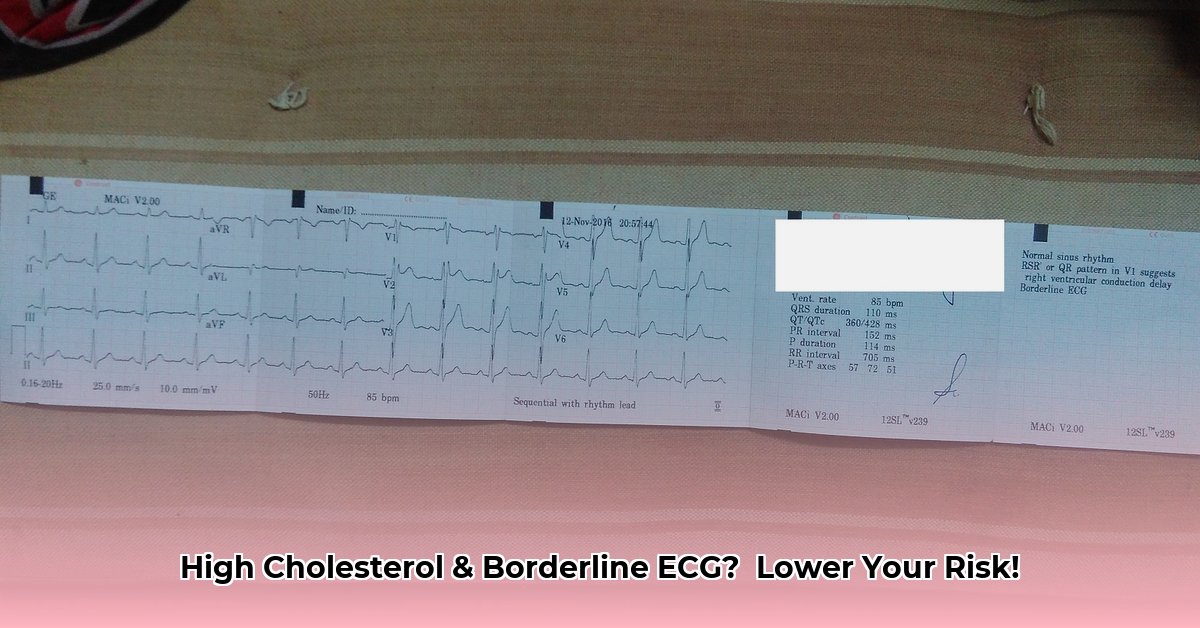
Got some slightly off-kilter heart readings (a borderline ECG) along with high cholesterol? Feeling a little lost and worried? You’re not alone. Lots of people face this, and it can be confusing to figure out what to do next. This guide is designed to help you understand what those results mean, how high cholesterol and a borderline ECG are connected, and what steps you can take to protect your heart. We’ll break down the medical jargon into plain English, give you practical tips for managing both conditions, and show you how to make smart choices to look after your heart health. We’ll even share insights from cardiologists to help you feel confident and in control. For more on borderline ECGs, see this helpful guide: [Borderline ECG info](https://www.mearnes.com/what-to-do-after-a-borderline-ecg).
Borderline ECG with High Cholesterol: Lowering Your Risk
Let’s talk about something a little concerning but also something you can definitely work on: that borderline ECG result and your high cholesterol. It sounds scary, but understanding these things is the first step to feeling better and reducing your risk of future heart problems.
Decoding Your Borderline ECG and Heart Health
An electrocardiogram (ECG) is a quick, painless test that records the electrical activity of your heart. It shows how your heart’s rhythm and electrical signals are working. A “borderline” result doesn’t automatically mean something’s seriously wrong. It means the ECG tracing shows some minor variations from the typical range, but these variations aren’t significant enough to confirm a definitive diagnosis. Think of it like a slightly blurry photo – the main picture is clear, but there are minor, subtle details that need a closer look. It might show some tiny irregularities in your heart rhythm or structure, things that might not even cause you any symptoms. Your doctor might want to do some more tests to make sure everything is okay, and that’s perfectly normal. Don’t panic – many people have borderline ECGs that turn out to be completely harmless.
High Cholesterol: The Silent Thief and Early Detection
High cholesterol is often called a “silent” condition because most people with high cholesterol don’t feel any different. It doesn’t usually cause noticeable symptoms until it leads to more serious problems. Cholesterol itself isn’t bad; your body needs it to build healthy cells. However, it’s the balance between different types of cholesterol that matters. Low-density lipoprotein (LDL), often called the “bad” cholesterol, is the troublemaker. This bad cholesterol can slowly damage your arteries, leading to the formation of plaque, a process called atherosclerosis. This plaque can narrow your arteries, reducing blood flow to your heart and brain, increasing your risk of heart attacks and strokes. The good news is that high cholesterol is often manageable. The key is to identify it early through a blood test and take steps to control it through lifestyle changes or medication.
The Double Whammy: Borderline ECG and High Cholesterol Together
Having both a borderline ECG and high cholesterol increases your chances of having heart problems compared to having either condition alone. It suggests your heart might be working a little harder than it should, and that there may be some underlying issues that need to be addressed. This extra work might be because of those cholesterol-related blockages in your arteries. The arteries are the pipes delivering blood to your heart, so if they’re partially clogged, your heart has to pump harder. That’s why it’s critical to tackle both issues simultaneously through a comprehensive approach involving lifestyle modifications, regular monitoring, and, if necessary, medication.
What Happens Next? Understanding Further Cardiovascular Investigation
If your doctor thinks you need further investigation, don’t worry, it’s standard procedure. They will likely order some more tests to get a clearer picture of your heart health and to determine the best course of action. These might include:
- A lipid panel: This blood test measures your different cholesterol levels – the good (HDL), the bad (LDL), and triglycerides. It gives your doctor a precise picture of your cholesterol profile and helps assess your risk of heart disease.
- More ECGs: Sometimes, a second or third ECG is done to confirm any patterns or changes seen in the first. This helps rule out any temporary factors that might have influenced the initial ECG results. Think of it as getting a second opinion or a closer look to rule out any inconsistencies.
- A stress test: This test assesses your heart’s performance under stress. During a stress test, you’ll exercise (usually on a treadmill or stationary bike) while your heart is monitored with an ECG.
- Echocardiogram: This test uses sound waves to create a moving image of your heart, showing its structure and function. It can help identify any abnormalities in your heart valves, chambers, or the way your heart muscle is contracting.
- Coronary Calcium Scan: A non-invasive CT scan that measures the amount of calcium in the arteries of your heart. Calcium is a marker of plaque buildup, so this scan can help assess your risk of heart disease.
Lifestyle Changes: Your Powerful Weapon for Heart Health
Before jumping to medication, lifestyle changes are your first line of defense against both high cholesterol and those borderline ECG findings. These changes can significantly reduce your risk and may even prevent the need for medication altogether. Here are some crucial ones:
- Diet Makeover: Eat a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins. Cut down on saturated and trans fats (found in many processed foods and fried items), cholesterol, sodium, and added sugars. Think of it as fueling your body with high-quality ingredients. The American Heart Association recommends limiting saturated fat to no more than 5-6% of your daily calories. Studies show that adopting a Mediterranean-style diet, which emphasizes fruits, vegetables, olive oil, and fish, can significantly reduce the risk of cardiovascular events.
- Get Moving: Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, or a combination of both. This could be brisk walking, jogging, swimming, cycling – anything that gets your heart rate up. Even short bursts of activity throughout the day can add up.
- Weight Management: Even a modest weight loss of just 5-10% of your body weight can greatly improve your cholesterol levels, blood pressure, and overall heart health. Losing weight also helps your body respond better to medication, if you end up needing it.
- Kick the Habit: Smoking is incredibly damaging to your blood vessels, making both high cholesterol and heart problems worse. Quitting smoking is one of the best things you can do for your overall health, and it has immediate and long-term benefits.
- Manage Stress: Chronic stress can contribute to high cholesterol and heart disease. Find healthy ways to manage stress, such as exercise, yoga, meditation, or spending time in nature.
Medication: A Supporting Role in Cholesterol Management
If lifestyle changes aren’t enough to get your cholesterol and ECG readings to where they should be, your doctor might suggest medication. Statins are a common and very effective type of medication for lowering LDL cholesterol. They work by blocking an enzyme in your liver that produces cholesterol. Other medications, such as ezetimibe, bile acid sequestrants, and PCSK9 inhibitors, may be used in combination with statins or as alternatives for people who can’t tolerate statins. Additionally, medications might be needed to manage specific heart rhythm issues highlighted by the ECG, depending on what those issues might be.
The Importance of Regular Check-Ups: Ongoing Monitoring and Early Detection
Regular check-ups with your doctor are crucial for monitoring your progress, making sure your treatment plan is working, and making adjustments as needed. Early detection and ongoing management are key to preventing serious cardiovascular problems. Don’t hesitate to ask your doctor any questions you have; understanding your condition empowers you to manage it and stay healthy. Consistent monitoring allows doctors to adjust treatment strategies promptly when necessary, leading to better outcomes.
Taking Control: Your Action Plan and Cardiac Wellness
Here’s a simple way to think about taking control:
| Stakeholder | Short-Term Goals | Long-Term Strategies |
|---|---|---|
| You | Diet and exercise changes, schedule those medical tests promptly. | Maintain healthy habits, attend regular check-ups, adhere to prescribed medication if necessary. |
| Your Doctor | Assess your overall cardiovascular risk, order further tests as needed, provide guidance on lifestyle modifications. | Monitor your progress, adjust treatment as needed based on test results and your response, offer ongoing support. |
Remember, this isn’t just something to worry about; this is something you can work proactively on to improve your health and well-being. By taking care of both your borderline ECG and high cholesterol, you’re taking a major step towards a healthier heart and a longer, more vibrant life. Early intervention is key— and remember to talk with your doctor to create a personalized plan that is right for you!
How to Interpret Borderline High Cholesterol Test Results
Key Takeaways:
- Borderline high cholesterol (200-239 mg/dL total cholesterol) isn’t a death sentence, but it signals increased long-term heart disease risk and warrants attention and proactive management.
- Lifestyle changes are your first line of defense and often can make a significant impact on your cholesterol levels. Diet, exercise, and weight management are crucial.
- Understanding your lipid panel (total cholesterol, LDL, HDL
- Top Rated Meditation Books to Deepen Your Practice - February 5, 2026
- Good Mindfulness Books For A Calmer, Happier Everyday Life - February 4, 2026
- Recommended Meditation Books for Beginners and Experienced Practitioners - February 3, 2026