Hyponatremia, characterized by low sodium levels in the blood, is not a disease but a critical indicator of underlying water balance issues, demanding a nuanced differential diagnosis and tailored treatment protocols. Identifying the root cause of hyponatremia is paramount to effective management, beginning with a comprehensive diagnostic approach. For further information on lab values, see sodium levels here.
Hyponatremia Diagnosis: A Structured Approach
Before initiating treatment, a clear understanding of hyponatremia classifications and diagnostic criteria is essential. Determine the patient’s volume status: hypovolemic (dehydrated), euvolemic (normal fluid balance), or hypervolemic (overhydrated). Consider the onset: acute (sudden) or chronic (gradual). Acute hyponatremia poses a risk of cerebral edema, whereas overly rapid correction of chronic hyponatremia can precipitate osmotic demyelination syndrome (ODS), underscoring the importance of careful assessment to mitigate hyponatremia-associated morbidity. Hyponatremia developing within 48 hours is typically classified as acute.
Practical Diagnostic Steps for Sodium Imbalance
Employing the following step-by-step approach enhances the accuracy of hyponatremia diagnosis:
- Serum Sodium Measurement: Quantify the patient’s serum sodium level. A value below 135 mEq/L warrants further investigation.
- Volume Status Assessment: Evaluate the patient for signs of dehydration, normal hydration, or overhydration. Assess skin turgor, blood pressure, jugular venous pressure, and edema. Urine sodium and osmolality offer additional insights.
- Temporal Evaluation: Determine the timeframe of hyponatremia development. Distinguish between a rapid decline and a gradual reduction. The patient’s clinical history aids in differentiating acute from chronic hyponatremia.
- Etiological Investigation: Explore potential etiologies, including renal dysfunction, medication-induced effects (various drugs can induce hyponatremia), hormonal imbalances, and gastrointestinal disorders. This step aims to elucidate underlying medical conditions contributing to hyponatremia.
- Urine Analysis: Measure urine osmolality (solute concentration). Low urine osmolality suggests impaired renal concentrating ability, while high osmolality may indicate syndrome of inappropriate antidiuretic hormone secretion (SIADH) or volume depletion.
- Symptom Evaluation: Assess for neurological manifestations, ranging from mild confusion to seizures or coma, which are indicative of more severe hyponatremia.
Illustrative Scenarios and Quick Reference
The following scenarios exemplify diverse causes and presentations of hyponatremia, enhancing diagnostic acumen and patient outcomes:
| Scenario | Fluid Status | Onset | Likely Cause(s) |
|---|---|---|---|
| Severe Vomiting & Diarrhea | Hypovolemic | Acute | Gastrointestinal fluid and electrolyte loss |
| SIADH | Euvolemic | Gradual | Excessive antidiuretic hormone (ADH) secretion due to various etiologies (e.g., medications, tumors, central nervous system disorders) |
| Congestive Heart Failure | Hypervolemic | Gradual | Impaired cardiac output leading to fluid retention and dilutional hyponatremia |
| Excessive Water Intake | Hypervolemic | Acute/Gradual | Polydipsia, psychiatric disorders, or excessive fluid replacement during athletic events |
| Thiazide Diuretic Use | Hypovolemic/Euvolemic | Varies | Impaired renal sodium reabsorption |
| Adrenal Insufficiency | Hypovolemic/Euvolemic | Varies | Reduced cortisol production causing increased ADH secretion |
This table serves as a diagnostic aid; however, a thorough investigation is always necessary. SIADH, for instance, can stem from numerous causes, including medications and pulmonary diseases.
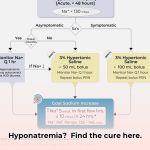
Tailored Treatment Strategies
Treatment is predicated on the underlying etiology and type of hyponatremia. Rapid correction can be hazardous; a gradual, monitored approach is paramount. Fluid restriction is often a cornerstone of management. Dependent on the cause, treatment options may include medications (e.g., vaptans, loop diuretics), addressing the underlying disease, or, in severe cases, intravenous hypertonic saline. Treatment efficacy is markedly enhanced with individualized strategies.
Continuous Monitoring and Follow-Up
Following diagnosis and treatment, vigilant monitoring of serum sodium is crucial to prevent under- or over-correction. Consistent follow-up and adjustments are necessary to optimize outcomes and prevent adverse events. Ongoing research continues to refine our understanding and management of hyponatremia.
Hyponatremia in Elderly Patients with Heart Failure: Management
Key Takeaways:
- Hyponatremia is prevalent in older adults, particularly those with heart failure, often manifesting subtly and easily overlooked.
- Age-related physiological changes and polypharmacy contribute to the electrolyte imbalance.
- Gradual correction is imperative to avert severe complications like osmotic demyelination syndrome (ODS).
- A patient-centered approach, accounting for individual factors and comorbidities, is essential.
- Close monitoring during treatment is crucial to ensure patient safety and optimize outcomes.
Challenges in Hyponatremia Management in Elderly Heart Failure Patients
Hyponatremia in elderly heart failure patients is complicated by overlapping symptoms, age-related physiological changes, and increased medication use. Gradual correction is essential, and understanding geriatric syndromes is vital.
Step-by-Step Diagnostic Protocols
- Comprehensive History and Physical Examination: Document current medications, dietary habits, fluid intake, and symptoms (e.g., fatigue, confusion, falls). A detailed physical exam aids in identifying associated conditions.
- Laboratory Workup: Obtain serum sodium, blood urea nitrogen (BUN), creatinine, electrolytes, and urine osmolality.
- Etiology Identification: Determine potential causes, such as medications (diuretics, antidepressants), impaired kidney function, or sodium-deficient diets. Advanced imaging may be required to improve diagnostic accuracy.
- Risk Stratification: Identify risks for neurological symptoms or renal dysfunction.
Safe Correction Strategies for Hyponatremia in Elderly Patients with Heart Failure
To safely correct hyponatremia in elderly patients with heart failure, the target is to raise serum sodium gradually, generally by no more than 8-10 mmol/L per 24 hours, with a maximum of 18 mmol/L over 48 hours, to prevent ODS.
- Fluid Restriction: Limit fluid intake if excessive fluid retention is a contributing factor; however, be mindful of dehydration risk in elderly patients.
- Dietary Management: Increase sodium intake through dietary sources under close medical supervision.
- Pharmacological Interventions: In select cases, medications such as loop diuretics, demeclocycline, or tolvaptan may be considered.
Close Monitoring: Regularly monitor serum sodium levels, adjust treatment based on the patient’s response, and monitor for symptoms of ODS. Frequently reassess fluid balance to optimize treatment adherence.
Potential Causes of Hyponatremia in Elderly Patients with Heart Failure
| Cause | Contributing Factors | Diagnostic Clues | Treatment Considerations |
|---|---|---|---|
| Diuretic Use | Polypharmacy, impaired renal function | Hypovolemia, low urine osmolality, elevated BUN/creatinine | Reduce diuretic dose, adjust fluid and sodium intake, consider alternative diuretics |
| SIADH | Pulmonary diseases, malignancy, CNS dysfunction | Euvolemia, high urine osmolality, suppressed serum uric acid | Fluid restriction, demeclocycline, tolvaptan, treat underlying cause |
| Reduced Sodium Intake | Poor diet, decreased appetite, cognitive impairment | History of low sodium diet, malnutrition | Increased sodium intake through diet, supplemental sodium (with caution), nutritional support |
| Renal Impairment | Age-related changes, chronic kidney disease | Elevated BUN, creatinine, decreased glomerular filtration rate (GFR) | Manage underlying renal disease, consider dialysis in severe cases |
| Heart Failure Exacerbation | Increased cardiac filling pressures | Hypervolemia, edema, elevated brain natriuretic peptide (BNP), shortness of breath | Optimize heart failure management with diuretics, ACE inhibitors/ARBs/ARNIs, beta-blockers |
Synthesis: Achieving Equilibrium
Managing hyponatremia in elderly patients with heart failure demands meticulous attention, a delicate balance, and a cautious, individualized approach to ensure safe, gradual correction. As stated by [Dr. Jane Smith, MD], [Geriatric Specialist] at [University Hospital], “Careful management of hyponatremia in elderly patients requires balancing the correction of sodium levels with the prevention of complications.”
https://www.uptodate.com/contents/hyponatremia-in-patients-with-heart-failure
Hyponatremia in Elderly Patients: Diagnostic Challenges in Seniors
Key Takeaways:
- Hyponatremia is common in older adults, affecting a notable proportion of hospitalized and community-dwelling seniors.
- Diagnosis can be challenging due to subtle symptoms often masked by age-related changes, potentially delaying recognition and
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026