Ever feel overwhelmed by medical codes? Understanding hyponatremia—low sodium in your blood—and its code, E87.1, can be tricky. This guide will walk you through everything you need to know to accurately diagnose and code hyponatremia, ensuring you get paid correctly for your work. We’ll break down the differences between hyponatremia and similar conditions, show you the step-by-step process of diagnosis, and give you the tools to confidently handle these cases. For more detailed ICD-10 information, see this helpful resource. Think of this as your cheat sheet to mastering hyponatremia—so you can focus on what matters most: your patients.
Understanding Hyponatremia, ICD-10 Code E87.1, and Differential Diagnoses
Let’s tackle hyponatremia—low sodium in your blood—and how to correctly code it (E87.1). It might sound complicated, but with a clear approach, it becomes much simpler. Getting the code right is crucial for proper billing and, more importantly, ensuring your patients get the best care. This guide walks you through the process, step by step. Learn ICD-10 coding for hyponatremia through easy-to-follow steps and expert insights, distinguishing it from similar conditions like SIADH and diabetes insipidus.
What is Hyponatremia? Recognizing Serum Sodium Levels & Osmolality
Imagine your body’s sodium levels are like the salt in a recipe: too little, and the dish tastes bland; too much, and it’s overwhelmingly salty. Hyponatremia occurs when blood sodium levels fall below 135 mmol/L (millimoles per liter). Sodium is a crucial electrolyte that helps regulate water balance, nerve impulses, and muscle contractions. This imbalance can cause various problems, from mild fatigue and nausea to serious neurological issues like seizures, coma, and even death. Code E87.1 specifically covers low sodium levels (hyponatremia) and low body fluid concentration (hypo-osmolality). Serum osmolality typically falls below 280 mOsm/kg in these cases.
Why is getting the code right so important? Because different causes of low sodium require different treatments, and proper coding ensures you get reimbursed accurately for your services. Moreover, accurate coding facilitates data collection for epidemiological studies and resource allocation. Hyponatremia affects millions worldwide and is particularly prevalent in elderly patients and those with chronic medical conditions. It is important to remember that hyponatremia is not always a primary diagnosis, but rather a manifestation of an underlying condition.
Diagnosing Hyponatremia: A Comprehensive, Step-by-Step Guide
Diagnosing hyponatremia is like solving a medical puzzle. You need to gather clues to figure out the full picture:
Step 1: The Patient’s Story – Anamnesis: Start by listening carefully to your patient. What symptoms are they experiencing? Common symptoms include nausea, headache, lethargy, confusion, muscle cramps, and, in severe cases, seizures or coma. Are they feeling unusually tired or weak? Do they have any headaches or muscle cramps? Are they taking any medications, especially diuretics (water pills), selective serotonin reuptake inhibitors (SSRIs), or certain pain medications? Knowing their medical history, including any kidney, heart, liver problems, or hormonal imbalances, is also vital. Ask about recent changes in fluid intake, including excessive water consumption.
Step 2: The Physical Check-up – Clinical Examination: A thorough physical exam is essential. Assess the patient’s vital signs, including heart rate and blood pressure. Look for signs that might indicate dehydration (hypovolemia), like dry mucous membranes, decreased skin turgor (elasticity), and orthostatic hypotension (a drop in blood pressure upon standing). Conversely, look for signs of fluid overload (hypervolemia), such as edema (swelling) in the extremities or pulmonary congestion (rales or crackles in the lungs). Pay close attention to their neurological function—are they confused, disoriented, weak, or experiencing any tremors or seizures?
Step 3: Lab Tests – Unmasking the Mystery: Laboratory tests are key to confirming the diagnosis and determining the underlying cause. These typically include:
- Serum Sodium Levels: This is the primary test, measuring the concentration of sodium in the blood. Levels below 135 mmol/L confirm hyponatremia.
- Serum Osmolality: This measures the concentration of particles in the blood. In hypo-osmolar hyponatremia (the most common type), serum osmolality is low (less than 280 mOsm/kg).
- Urine Sodium: This test helps determine if the kidneys are appropriately conserving sodium or losing too much.
- Urine Osmolality: This helps assess the kidney’s ability to concentrate urine.
- Complete Metabolic Panel (CMP): This provides information about kidney function, liver function, and glucose levels, which can help identify potential causes of hyponatremia.
- Thyroid Function Tests: Hypothyroidism can cause hyponatremia.
- Cortisol Level: Adrenal insufficiency can also lead to hyponatremia.
- Arginine Vasopressin (AVP) Level: In some cases, measuring AVP levels can help diagnose SIADH.
The results of these tests provide crucial information about whether the body is holding onto or losing too much fluid and whether the kidneys are functioning properly. Depending on the patient’s condition, further tests like a chest X-ray (to look for lung abnormalities that could cause SIADH) or a water deprivation test (to diagnose diabetes insipidus) may also be needed. The timing of these tests after admission is crucial for capturing transient changes in sodium levels, especially in acute settings.
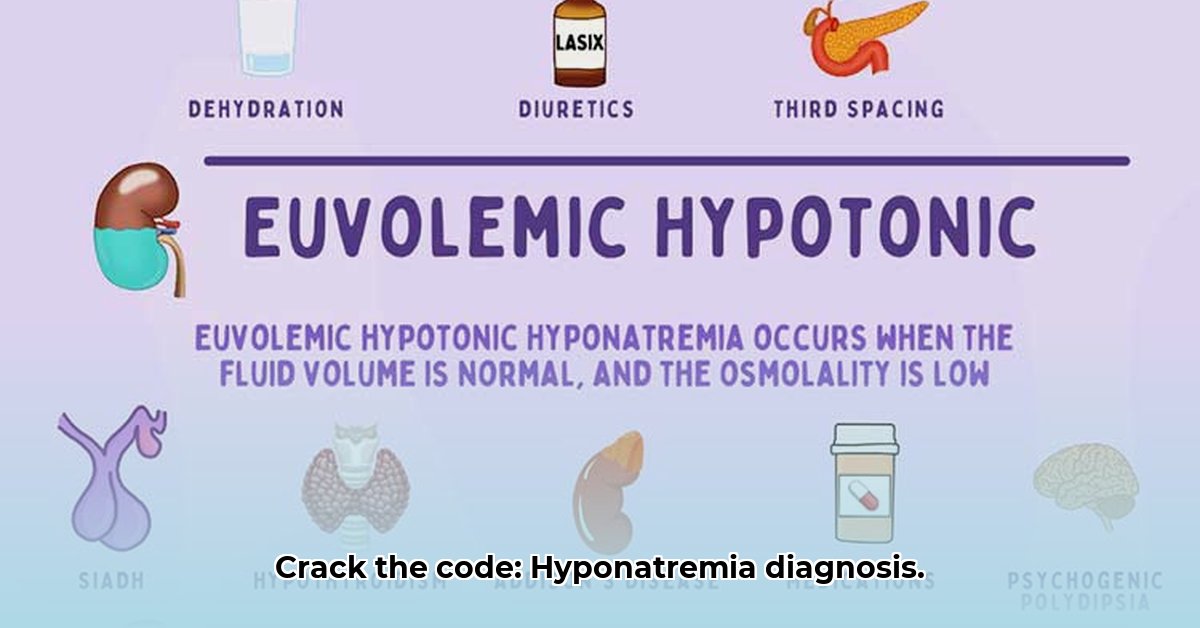
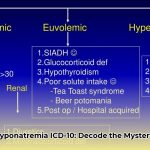
Step 4: Putting the Pieces Together – Classifying the Hyponatremia: Based on the information gathered, you’ll need to classify the patient’s hyponatremia. This isn’t merely about the sodium number; it’s about the bigger picture. There are three main types, classified according to the patient’s volume status:
- Hypovolemic Hyponatremia: The body has lost both sodium and water, but proportionally more sodium has been lost, resulting in a lower sodium concentration. Causes include vomiting, diarrhea, excessive sweating, diuretic use, and adrenal insufficiency. Urine sodium levels are typically low (less than 30 mEq/L) if the kidneys are functioning properly and trying to conserve sodium. However, in cases of diuretic use or salt-wasting nephropathy, urine sodium levels may be elevated.
- Euvolemic Hyponatremia: The total body water is normal, but the sodium is diluted. This often occurs in conditions like SIADH (Syndrome of Inappropriate Antidiuretic Hormone secretion), hypothyroidism, glucocorticoid deficiency, and psychogenic polydipsia (excessive water drinking). Urine sodium levels are variable but often greater than 20 mEq/L in SIADH.
- Hypervolemic Hyponatremia: The body has too much fluid overall, including excess water that dilutes the sodium levels. This might be seen in heart failure, kidney disease (especially nephrotic syndrome), and liver cirrhosis. Patients typically exhibit signs of fluid overload, such as edema and pulmonary congestion. Urine sodium levels are typically low (less than 20 mEq/L) as the kidneys try to retain sodium.
Differential Diagnosis: Distinguishing Hyponatremia from Similar Conditions
Hyponatremia isn’t the only condition that can cause low sodium. It’s vital to distinguish it from similar issues, particularly SIADH and diabetes insipidus, as well as adrenal insufficiency and cerebral salt wasting. Here’s a simplified comparison:
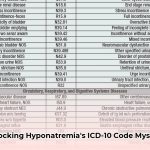
| Feature | Hyponatremia (E87.1) | SIADH (E22.2) | Diabetes Insipidus (E23.2) | Adrenal Insufficiency | Cerebral Salt Wasting |
|---|---|---|---|---|---|
| Blood Sodium | Low (<135 mmol/L) | Typically low | Can vary; often normal or slightly low | Low | Low |
| Blood Osmolality | Low | Low | Usually high | Low | Low |
| Urine Concentration | Varies, depends on the type of hyponatremia | High | Low | Varies | Varies |
| Urine Sodium | Varies, depends on the type of hyponatremia | Often high (though can be low if sodium intake is restricted) | Often low | High | High |
| Volume Status | Can be hypovolemic, euvolemic, or hypervolemic | Euvolemic or slightly hypervolemic | Hypovolemic if fluid intake is inadequate to keep up with urinary losses; can be euvolemic with adequate fluid intake |
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026