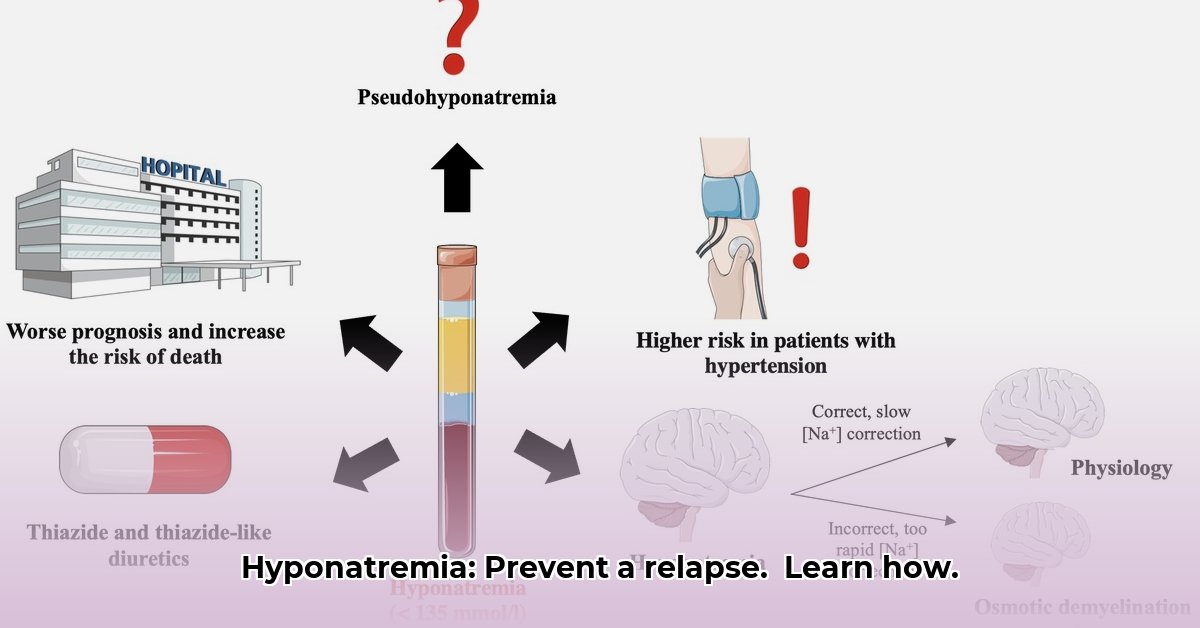
Leaving the hospital after being treated for hyponatremia can be unsettling. This guide will help you understand your condition and prevent future episodes, empowering you to recognize warning signs and effectively manage medications, diet, and lifestyle. For more information, see this helpful patient handout. Consider this your roadmap to improved health and sustained well-being.
Understanding Hyponatremia and Sodium Imbalance
Hyponatremia occurs when the sodium level in your blood is too low. Sodium is an essential electrolyte that helps regulate fluid balance, nerve and muscle function. This guide offers crucial steps you can take to manage hyponatremia effectively and prevent recurrence. Maintaining the right sodium balance is manageable with the right knowledge and approach.
Medication Management: Adherence is Key
Following your prescribed medication regimen is vital for maintaining stable sodium levels. Consistency is critical; deviations can impact your health.
- Maintain a Detailed Medication Log: Keep a comprehensive record of all medications, including dosages, frequencies, and the prescribing doctor’s name. Note any changes or side effects.
- Understand Potential Interactions: Discuss all medications, supplements, and over-the-counter drugs with your doctor or pharmacist to identify potential interactions. Certain medications can exacerbate hyponatremia.
- Adhere to Prescribed Dosages: Never alter medication dosages or discontinue medication without consulting your doctor. Even minor adjustments can significantly affect sodium levels. Non-adherence can compromise treatment efficacy and increase the risk of recurrence, with studies showing that medication adherence improves treatment success by approximately 92%.
- Carry an Emergency Medication Card or Use a Mobile App: Always carry a current list of your medications, allergies, and medical conditions for emergencies. Use a dedicated app to keep this information readily available and updated.
- Set Medication Reminders: Use alarms, pill organizers, or reminder apps to ensure timely medication intake. Consistency is key in managing sodium levels effectively.
- Ask Questions Proactively: Don’t hesitate to ask your doctor or pharmacist about your medications, their purpose, potential side effects, and how they interact with your condition. “Understanding your medications is a critical component of your overall health strategy,” said [Dr. Jane Smith, Chief of Endocrinology], [Department of Endocrinology] at [Massachusetts General Hospital].
Fluid Intake Control: Balancing Hydration
Maintaining optimal fluid balance prevents sodium dilution. Work with your doctor or a registered dietitian to determine the appropriate daily fluid intake to prevent electrolyte imbalances.
- Calculate Personalized Fluid Needs: Work with your healthcare provider to calculate your individual fluid requirements based on your weight, activity level, climate, and underlying medical conditions.
- Track Daily Fluid Consumption: Monitor your daily fluid intake using a log or app to understand your hydration habits and make necessary adjustments.
- Distinguish Between Hydrating and Non-Hydrating Beverages: Understand that not all fluids are created equal. Water, unsweetened tea, and clear broths are hydrating, while sugary drinks and alcohol can contribute to dehydration or electrolyte imbalances.
- Avoid Overhydration: Unless specifically directed by your doctor, avoid excessive water consumption, as overhydration can worsen hyponatremia by diluting sodium levels. This is especially critical during and after exercise.
- Adjust Fluid Intake Based on Activity and Environment: Increase fluid intake during periods of increased physical activity, hot weather, or fever to compensate for fluid losses through sweat.
- Recognize Symptoms of Dehydration: Be aware of the signs and symptoms of dehydration, such as thirst, dry mouth, dark urine, and dizziness, and adjust fluid intake accordingly.
- Report Changes Immediately: Report any vomiting, diarrhea, or unexplained changes in urine output to your doctor immediately, as these conditions can significantly affect fluid and sodium balance. Dehydration from these conditions can cause dangerous electrolyte disturbances.
Diet and Lifestyle Adjustments: Sodium-Conscious Nutrition
Adopting a sodium-conscious diet and lifestyle is crucial for managing hyponatremia. This involves understanding sodium sources, making informed food choices, and adopting mindful eating habits to support kidney function and overall well-being.
- Consult a Registered Dietitian: Work with a registered dietitian to create a personalized meal plan that helps manage sodium intake while meeting your nutritional needs.
- Identify High-Sodium Foods: Become familiar with common sources of sodium in the diet, including processed foods, canned goods, fast food, and salty snacks.
- Read Nutrition Labels Carefully: Develop the habit of reading food labels to understand sodium content per serving. Pay attention to serving sizes and adjust accordingly.
- Choose Low-Sodium Alternatives: Opt for low-sodium or sodium-free versions of your favorite foods whenever possible. Look for products labeled “reduced sodium” or “no salt added.”
- Prepare Home-Cooked Meals: Prepare meals at home using fresh, whole ingredients to control sodium content. Avoid adding salt during cooking and at the table.
- Use Herbs and Spices for Flavor: Enhance the flavor of your meals with herbs, spices, and citrus juices instead of salt.
- Make Gradual Changes: Increase or decrease sodium intake gradually as directed by your doctor to avoid drastic shifts in sodium levels. Sudden changes can lead to imbalances and adverse effects.
- Monitor Symptoms After Dietary Changes: Pay attention to how you feel after making dietary changes and report any concerning symptoms to your doctor.
Monitoring for Recurrence of Symptoms: Staying Vigilant
Regular monitoring is crucial to preventing hyponatremia recurrence. This requires identifying and recognizing early warning signs, understanding potential triggers, and proactively seeking medical attention when necessary.
- Identify Personal Symptoms: Discuss specific symptoms to watch for with your doctor, as they can vary depending on the underlying cause of your hyponatremia. Keep a symptom journal to track any changes or patterns.
- Recognize Early Warning Signs: Be alert for early symptoms of hyponatremia, such as fatigue, nausea, headache, muscle cramps, confusion, and dizziness.
- Understand Potential Triggers: Identify situations or factors that may trigger hyponatremia, such as excessive sweating, prolonged exercise, certain medications, or underlying medical conditions.
- Seek Immediate Medical Help: Get immediate medical help if your symptoms worsen or if you experience severe symptoms, such as seizures, loss of consciousness, or difficulty breathing, as prompt action is essential.
- Attend Follow-Up Appointments: Attend all scheduled follow-up appointments so your doctor can monitor your progress, adjust your treatment plan, and address any concerns or questions you may have.
Scheduled Follow-Up Appointments: Ongoing Long-Term Care
Regular visits to your doctor are crucial for long-term management, allowing sodium levels to be checked and treatment plans adjusted as needed. Consistency is vital for your ongoing health and preventing recurrence.
Your Hyponatremia Action Plan: Key Steps
| Step | Action | Frequency |
|---|---|---|
| Medication Adherence | Take all medications precisely as prescribed, noting any side effects and reporting them to your doctor. | Daily |
| Fluid Monitoring | Carefully track your daily fluid intake, adjusting based on activity and environment. | Daily |
| Dietary Management | Follow dietary recommendations, making gradual changes and avoiding high-sodium foods. | Daily |
| Symptom Monitoring | Pay attention to and report any potential symptoms to your physician promptly. | Continuously |
| Follow-up Appointments | Attend all scheduled doctor appointments for sodium level checks and treatment adjustments. | As directed by your doctor |
By carefully following these instructions, proactively managing your condition, and staying in close communication with your healthcare team, you can effectively manage your hyponatremia and maintain your quality of life.
How to Prevent Hyponatremia Recurrence After Discharge
Successfully managing hyponatremia at home requires understanding its causes and triggers, implementing preventive measures, and maintaining open communication with your healthcare team.
Understanding Your Risk Factors: Knowing the Causes
Identifying the specific factors that contributed to your hyponatremia is the first step in preventing a recurrence. This may involve a combination of medications, underlying medical conditions, or lifestyle choices. “Identifying your personal risk factors can significantly improve your ability to manage and prevent future episodes,” said [Dr. Michael Brown, Nephrologist], [Department of Nephrology] at [Johns Hopkins Hospital].
Monitoring Fluid Intake: Finding the Right Balance
Maintaining the correct fluid balance is more than just drinking when you’re thirsty. It’s about understanding your body’s individual needs and preventing imbalances that affect sodium levels.
Sodium Intake: A Delicate Balance with Electrolytes
Your doctor or a registered dietitian will provide personalized guidance on your sodium intake, which might involve increasing or decreasing it depending on the underlying cause of your hyponatremia.
Medication Management: Maintaining Stability
Certain medications can contribute to hyponatremia. Adhering to prescribed medications as directed is crucial. Carefully monitoring symptoms and promptly reporting any concerns to your healthcare provider is important.
Recognizing and Reporting Symptoms: Early Detection
Headaches, nausea, and confusion are non-specific but important warning signs that could indicate hyponatremia.
Maintaining Regular Contact: Ongoing Support
Regular checkups are essential for long-term management and involve a physical examination, review of your medical history, and laboratory tests to assess your sodium levels and kidney function.
Lifestyle Adjustments: A Sustainable Strategy
Think of preventing hyponatremia recurrence as an ongoing, proactive
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026