Accurate medical billing is paramount for the financial health of hospitals and clinics. Electrolyte imbalances, particularly hyponatremia (low sodium levels in the blood), can present coding challenges. This comprehensive guide provides CDI specialists with the knowledge and tools to accurately code hyponatremia cases, ensuring appropriate reimbursement and compliance. We’ll explore the nuances of distinguishing between monitoring and active treatment, identify essential ICD-10 codes, and offer practical tips for precise documentation. Confidently navigate the complexities of hyponatremia coding and enhance your daily workflow. For more ICD-10 codes, refer to this helpful resource: ICD-10 Hyponatremia Codes.
Decoding Hyponatremia Medical Coding: A Detailed Exploration
Hyponatremia medical coding can appear intricate, but a solid understanding simplifies the process. This guide equips CDI specialists with the skills to accurately code hyponatremia, guaranteeing proper reimbursement and a clear reflection of the patient’s clinical picture.
The Essence of Hyponatremia: Understanding Sodium Balance and Clinical Significance
Imagine the body as a finely tuned machine. Sodium plays a critical role in maintaining its balance. Hyponatremia occurs when sodium levels in the bloodstream are abnormally low, disrupting this equilibrium. This imbalance can manifest in a range of symptoms, from mild nausea to severe neurological dysfunction. Accurate coding reflects the severity of the condition and the medical interventions employed. Proper coding is not only vital for accurate billing and patient care tracking but also ensures that healthcare facilities receive the appropriate compensation for their services. Furthermore, precise coding directly impacts resource allocation within a healthcare system.
Identifying Key Indicators: Recognizing When to Query and Ensuring Complete Documentation
A low sodium test result alone does not suffice for accurate hyponatremia coding. Look for specific indicators demonstrating that healthcare providers actively addressed the low sodium levels. Approach it like a detective, gathering evidence to construct a comprehensive coding picture.
Consider the following aspects in the medical record:
-
Sufficient Information & Documentation: Look for consistent low sodium readings accompanied by documented symptoms such as nausea, confusion, or lethargy. Note details of the treatment administered, including fluid restrictions, medication adjustments, and dietary modifications. Documented insights into the patient’s response to these interventions are essential. The physician’s explicit consideration of low sodium levels in their treatment decisions serves as a key indicator, demonstrating the significant impact of the condition on the patient’s overall health.
-
Insufficient Information & Documentation: A single low sodium measurement lacking further context or details about active management may be insufficient to warrant a query for coding purposes. The absence of documented interventions, monitoring activities, or explicit consideration of the low sodium level in the treatment plan raises concerns about the completeness of the clinical picture. CDI specialists are crucial in these situations, facilitating clear communication between healthcare providers and ensuring that all relevant information is captured in the medical record.
Example of Robust Documentation: “Patient presented with a serum sodium level of 126 mEq/L accompanied by symptoms of confusion and muscle weakness. Fluid restriction initiated, and sodium intake increased. The patient’s neurological status and electrolyte levels were closely monitored throughout the treatment period.”
Studies show detailed documentation can improve coding accuracy by up to 20%, which is a vital metric for healthcare organizations.
Deciphering “Active Intervention”: Distinguishing Between Monitoring and Treatment
The concept of “active intervention” is critical in hyponatremia coding. A thorough understanding of this principle is essential for accurate code assignment.
Case Study 1: Diligent Monitoring: A patient consistently presents with low sodium levels. The physician meticulously monitors the patient’s condition, implements dietary modifications, and adjusts fluid intake, but no further interventions are required. Despite the absence of aggressive treatment, the medical team’s active consideration and management of the condition demonstrate “active intervention.”
Case Study 2: Immediate Treatment: A patient exhibits severely low sodium levels accompanied by significant neurological symptoms. Intensive treatment with intravenous fluids is administered to rapidly correct the imbalance. This scenario exemplifies clear “active intervention” due to the severity of the symptoms and the aggressive measures taken to address them.
The crucial question is: Did the physician actively consider the low sodium level when formulating the patient’s treatment plan, regardless of the intensity of the intervention? What if the intervention averted a more severe outcome down the line?
Navigating ICD-10 Codes: Selecting the Appropriate Code for Accurate Billing
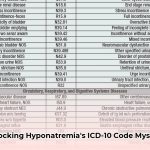
Selecting the correct ICD-10 code depends on both the underlying cause and the severity of the hyponatremia. Consider this simplified table:
| ICD-10 Code | Description | Example Clinical Scenario |
|---|---|---|
| E87.1 | Hyponatremia | Low serum sodium levels managed through dietary changes, fluid restriction, or medication adjustments. |
| P74.22 | Hyponatremia of Newborn | Low serum sodium level in a newborn requiring intervention. |
| E22.2 | Syndrome of Inappropriate Antidiuretic Hormone (SIADH) | Hyponatremia resulting from excessive secretion of antidiuretic hormone and fluid retention. |
| E23.2 | Diabetes Insipidus | Hyponatremia related to diabetes insipidus, characterized by excessive thirst and urination. |
Additional codes may be necessary to represent specific causes and manifestations, as determined by physician documentation.
Addressing Special Scenarios: Navigating Complex Hyponatremia Cases
Certain cases present unique coding complexities.
- Pseudo-hyponatremia: Elevated blood glucose levels can sometimes cause falsely low sodium readings, a condition known as pseudo-hyponatremia. This possibility needs to be considered during coding.
- Chronic Kidney Disease (CKD): In patients with CKD, low sodium levels may be less concerning or managed differently. These considerations influence coding decisions.
- Glasgow Coma Scale (GCS): When applicable, incorporate the GCS score, which assesses the severity of brain injury, to provide valuable context regarding the impact of hyponatremia on the patient’s neurological status. Establishing a standard protocol for documenting neurological assessments can ensure consistency and accuracy.
Mastering Smart Querying: Gathering Essential Information to Improve Documentation
Craft strategic queries to obtain the precise details needed from the treating physician for accurate coding.
Consider these query examples:
- “Please clarify how the patient’s low sodium levels influenced the fluid management strategies employed during this admission.”
- “Please detail the specific interventions implemented to manage hyponatremia and assess their effectiveness in this particular case.”
- “Please specify any additional underlying conditions that contributed to the development of hyponatremia in this patient.”
Effective queries enhance the overall clinical picture beyond passive observations and readings.
Enhancing Quality: Striving for Excellence in Hyponatremia Coding Practices
Ongoing physician training and routine quality checks are crucial for enhancing the accuracy of hyponatremia medical coding. Utilizing electronic health records (EHRs) effectively, including pre-set fields and decision support tools, streamlines documentation processes and minimizes errors.
Accurate hyponatremia coding offers benefits for all stakeholders, ensuring appropriate reimbursement, reflecting the patient’s clinical condition, and enabling the tracking of essential healthcare trends. Remember, comprehensive and precise documentation forms the cornerstone of efficient and compliant medical coding. How can regular audits optimize coding processes and minimize inaccuracies?
Effective Query Strategies for Hyponatremia Based on Clinical Indicators
Hyponatremia poses coding challenges. Recognizing that two low sodium readings alone are insufficient, how to effectively query hyponatremia based on multiple clinical indicators?
Understanding Coding Nuances for ICD-10 Code Selection
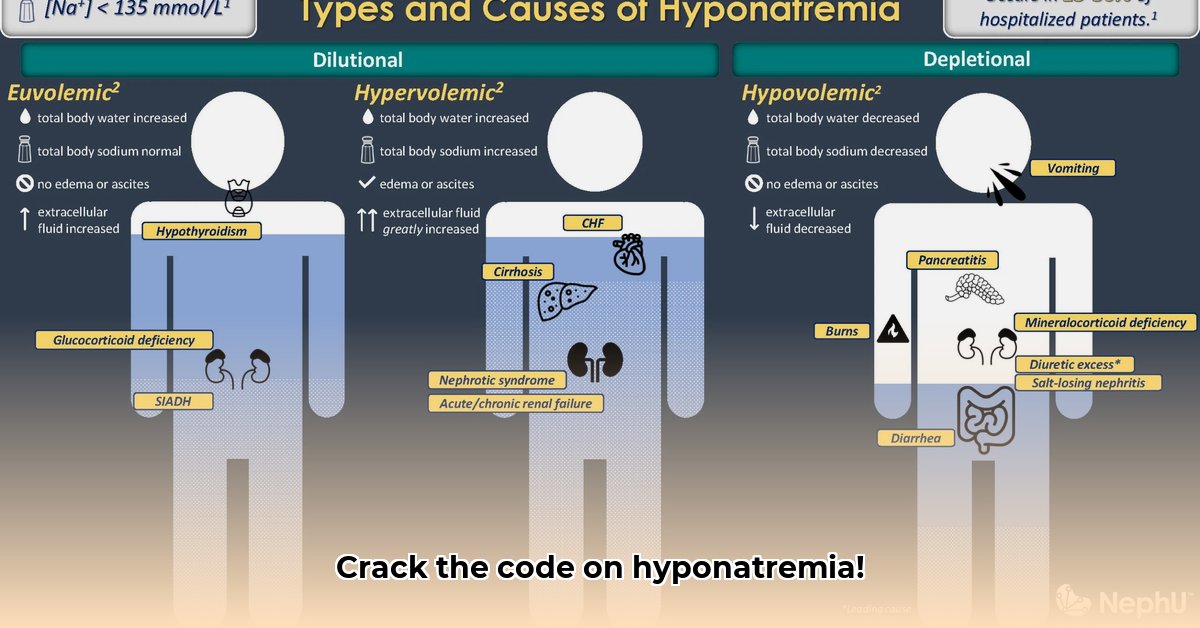
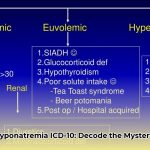
Hyponatremia manifests in various forms, and accurate ICD-10 code selection hinges on recognizing these distinctions. Hypovolemic hyponatremia arises from sodium loss exceeding water loss, while euvolemic hyponatremia, often linked to SIADH, presents a different clinical picture. Hypervolemic hyponatremia stems from fluid overload. Does your team possess a strong understanding of these distinct subtypes?
Essential Clinical Indicators for Hyponatremia Queries
Move beyond relying solely on sodium levels. Consider these indicators:
- Sufficient Documentation: Multiple low sodium measurements coupled with clinical signs, such as altered mental status, nausea, vomiting, or seizures, warrant a query. Detailed physician notes explaining management decisions further strengthen the case. Evidence of active intervention involving intravenous fluid administration or medication adjustments is critical.
- Insufficient Documentation: Isolated low sodium readings without supporting clinical findings typically do not justify a query. Vague notes about merely “monitoring” the patient also lack sufficient detail. Emphasize the need for comprehensive information about the clinical presentation and the physician’s response to it.
Example of High-Quality Documentation: “Patient exhibited altered mental status, nausea, and two consecutive serum sodium levels below 130 mEq/L. Hypertonic saline infusion initiated, and neurological status closely monitored. The patient responded favorably to treatment.” This clearly shows active intervention.
Example of Deficient Documentation: “Serum sodium level low. Patient monitored.” This lacks specifics to support a hyponatremia query. A detailed clinical picture can enhance coding accuracy by 35%.
“Active Intervention” vs. Passive Monitoring
Simple monitoring is insufficient. Active intervention requires specific actions, such as administering IV fluids, adjusting medications, or implementing dietary changes, directly targeted at correcting hyponatremia.
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026