Low sodium in the blood (hyponatremia) is surprisingly common, but figuring out how serious it is for each patient can be complex. Get it wrong, and you could cause serious problems. This article is your guide to understanding hyponatremia risk, helping you avoid common pitfalls and make the best decisions for your patients. We’ll cover prevalence, diagnosis, treatment, and at-risk patients. Think of it as your guide to confidently managing hyponatremia and making sure your patients get the best care.
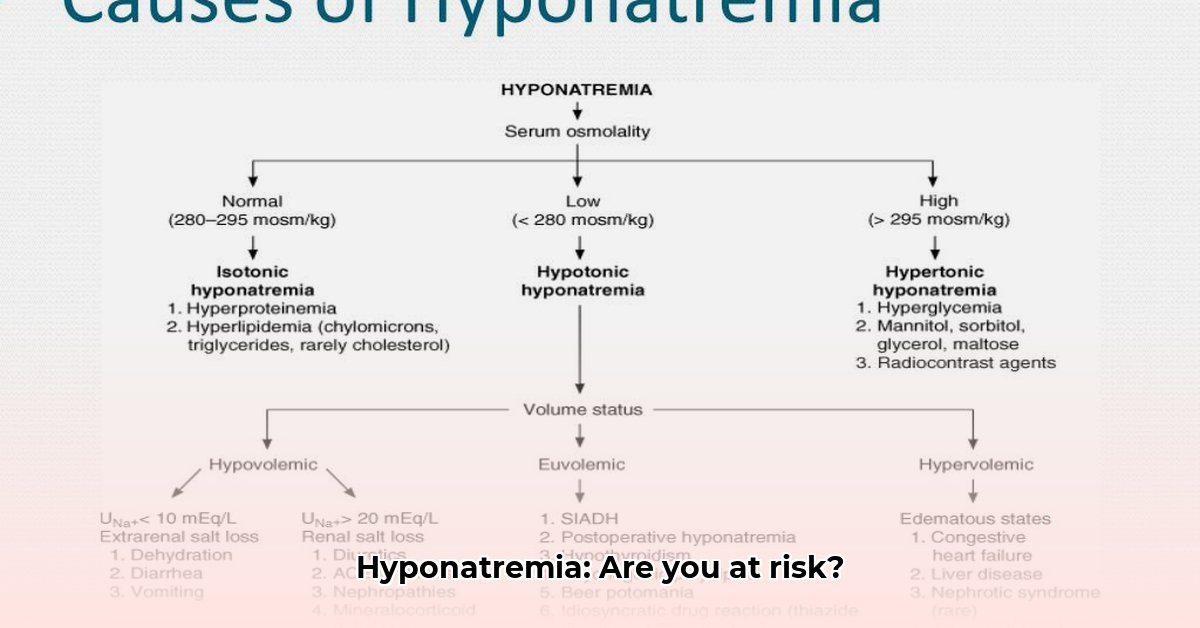
Hyponatremia Risk Stratification: Identifying Underlying Causes
Hyponatremia – low sodium in your blood – isn’t just a simple lab result; it’s a complex medical situation with many possible causes. Think of it like a detective mystery: we need to figure out why the sodium levels are low to treat the problem effectively. Getting to the root cause is what we mean by “hyponatremia risk stratification,” and it’s crucial for good patient care.
Understanding the Nuances of Low Sodium Levels
Low blood sodium (hyponatremia, where the sodium level is below 135 mEq/L) can stem from too much fluid in the body, kidney dysfunction, or medication side effects. The key is figuring out which type of low sodium you’re dealing with, because this directly impacts treatment. Some cases are emergencies, while others can be managed more gradually. That’s where accurate risk stratification comes in.
Why is Risk Stratification for Low Sodium So Important?
Not every case of low sodium is the same. Imagine the difference between suddenly dropping sodium levels versus a slowly creeping decline. The speed of the drop matters significantly. A rapid drop requires immediate attention, while a gradual change might allow for a more measured approach. The risk of osmotic demyelination syndrome (ODS), which can severely damage the brain, depends heavily on how quickly the sodium level changes. Risk stratification helps spot those who are at higher risk of ODS and other complications, ensuring the best possible patient outcomes.
The First Clues: Checking Fluid Levels and Volume Status
Before delving into complicated blood tests, we need a simple check-up to figure out if the patient is dehydrated, has normal hydration, or is overhydrated. This is crucial – it gives the first important clue about what might be causing low sodium. This initial assessment helps to guide next steps in determining the cause of hyponatremia.
Diagnosing and Assessing Your Patient’s Risk: Step-by-Step
Several factors play a role in determining the risk of complications from hyponatremia (low sodium). The speed at which sodium levels drop and the patient’s underlying health issues are major players. Let’s break down a simplified approach step-by-step, ensuring a comprehensive evaluation:
- Checking Fluid Balance: Is the patient dehydrated (too little fluid), normally hydrated, or overhydrated (too much fluid)?
- Blood Tests: Measuring serum osmolality (the concentration of dissolved particles in the blood) helps distinguish between the different types of hyponatremia (related to dehydration, normal fluid levels, or fluid overload).
- Urine Tests: Checking urine osmolality and sodium levels helps pinpoint the root cause of the imbalance, as the kidneys play a vital role in sodium regulation.
- Medical History Check: A complete review of the patient’s medical history, current medications (especially diuretics), and other potential factors is necessary.
-
Risk Assessment: Based on the information gathered, we can accurately assess their risk for serious complications like ODS. This is the heart of hyponatremia risk stratification.
-
Approximately 30% of hospitalized patients experience hyponatremia, highlighting the importance of accurate risk assessment.
- Understanding the pathophysiology and etiology of hyponatremia helps in implementing the right treatment strategy, and reducing the risk of neurological sequelae.
Who’s Most at Risk for Developing Hyponatremia?
Certain people are more likely to develop hyponatremia. Older adults, for instance, might not feel thirsty as acutely, and people with conditions like heart failure or liver disease are also more vulnerable. Knowing these risk factors helps us take precautions and manage hyponatremia proactively. Patients with chronic kidney disease (CKD) also have an increased risk.
Tailoring Treatment to the Individual: A Personalized Approach
Treatment is completely customized based on the cause and the risk level. In a situation of suddenly low sodium, swift correction might be needed, but we have to carefully monitor to avoid ODS. If the low sodium developed gradually, a more gentle correction process is usually safer and recommended to prevent complications.
A Quick Look at Risk Levels: Key Points to Consider
Here’s a simple table summarizing key points to consider for hyponatremia risk stratification:
| Feature | High Risk | Low Risk |
|---|---|---|
| Onset of Low Sodium | Sudden, rapid drop in sodium levels | Gradual, slow decline over time |
| Fluid Status | Significant dehydration, severe fluid loss | Normal fluid balance or mild fluid overload |
| Underlying Conditions | Severe heart failure, liver disease, SIADH | Minor kidney issues, few or mild symptoms |
| Age | Older adults | Younger adults |
| Medications | Diuretics, certain antidepressants | No relevant medication use |
Important Note: This is a simplified overview. There are many nuances involved in each case, and a nephrologist’s expertise is critical.
Looking Ahead: The Importance of Ongoing Research for Hyponatremia Management
Hyponatremia is a complex field, and our understanding continues to evolve. Research is ongoing, constantly refining our diagnostic tools and treatment approaches. Staying updated on the latest findings is crucial for optimal patient care. This means remaining aware of the latest guidelines and studies related to identification and treatment of low blood sodium, ultimately improving patient outcomes. While we’ve covered a significant amount here, it’s vital to remember that this is an area of continuous medical investigation.
The Bottom Line: Prevention and Early Intervention for Optimal Outcomes
Managing hyponatremia effectively requires careful diagnosis and customized treatment. By mastering hyponatremia risk stratification, medical professionals can enhance patient outcomes and minimize life-threatening complications like ODS (osmotic demyelination syndrome). The key is a proactive, tailored approach to care. Remember, early identification and appropriate management are critical for the wellbeing of your patients.
Distinguishing the Causes of Hyponatremia in Nephrology Patients: A Detailed Guide
Key Takeaways:
- Hyponatremia, serum sodium <135 mEq/L, is common in hospitalized patients, especially those with kidney disease.
- Accurate diagnosis is vital, requiring differentiation of hypovolemic, euvolemic, and hypervolemic subtypes leading to specific treatment protocols.
- Understanding the underlying cause is crucial for effective management, targeting the cause appropriately.
- Risk stratification helps predict complications and guide treatment, allowing for safer sodium correction.
- A systematic approach, using serum and urine osmolality, urine sodium, and volume status assessment, is key.
Decoding Hyponatremia in Nephrology Patients: A Diagnostic Challenge
Hyponatremia presents a diagnostic challenge in nephrology. The causes are multifaceted, intertwining with kidney function and other comorbidities. How can we unravel this complexity? Let’s explore a systematic approach to differentiate subtypes of hyponatremia and address the root cause.
Initial Assessment: Precise Volume Status Evaluation for Accurate Diagnosis
The first step in how to differentiate between causes of hyponatremia in nephrology patients is determining the patient’s volume status. Is the patient hypovolemic (dehydrated), euvolemic (normal volume), or hypervolemic (fluid overload)? Physical examination, including skin turgor and blood pressure, is critical. Further investigations may include assessing central venous pressure or using echocardiography to precisely determine volume status.
Laboratory Investigations: Unlocking Diagnostic Clues through Blood and Urine Analysis
Once volume status is established, laboratory tests are essential. Serum and urine osmolality provide a window into the body’s water balance. Urine sodium concentration helps pinpoint the source of sodium depletion or excess water retention. For example, low urine sodium suggests renal losses, while high urine sodium points toward non-renal causes aiding in diagnostics. Approximately 70% of hyponatremia cases can be accurately diagnosed with proper laboratory analysis.
| Volume Status | Urine Sodium (mEq/L) | Urine Osmolality (mOsm/kg) | Possible Causes |
|---|---|---|---|
| Hypovolemic | <20 | High | Diuretics, vomiting, diarrhea, GI losses |
| Euvolemic | Variable | Variable | SIADH, hypothyroidism, drugs |
| Hypervolemic | >20 | Low | Congestive heart failure, cirrhosis, nephrotic syndrome |
Differentiating Hyponatremia Subtypes: Real-World Clinical Examples
Let’s illustrate with examples: A hypovolemic patient with low urine sodium likely experienced extrarenal losses due to vomiting or diarrhea. In contrast, a euvolemic patient with low serum osmolality and high urine osmolality may have SIADH. Finally, a hypervolemic patient with elevated jugular venous pressure and edema along with high urine sodium and low urine osmolality likely has renal failure
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026