judulcuy: “Spot Low Sodium Symptoms in Elderly: Expert Guide”
bahasaart: “en-US”
formatart: “informational article with instructional guide elements”
kabeh: “All data from the draft article has been used.”
Spot Low Sodium Symptoms in Elderly: Expert Guide
Low sodium, or hyponatremia, can be a subtle but serious health issue in older adults. Often, it doesn’t present with obvious symptoms, making it essential to be aware of potential signs. This expert-guided article provides a comprehensive understanding of low sodium in seniors, emphasizing the importance of accurate diagnosis and safe management. We will explore the challenges of identifying symptoms, the critical role of caregivers, and effective strategies for prevention. Understanding these factors can significantly improve the health and well-being of elderly individuals under your care. Are you ready to recognize the often-overlooked signs of hyponatremia and take proactive steps to safeguard the health of the seniors you support? For more information on hyponatremia symptoms, see this helpful resource: Hyponatremia symptoms.
Understanding Low Sodium (Hyponatremia) in the Elderly
Hyponatremia awareness; early detection; elderly care; sodium imbalance
Hyponatremia, a condition characterized by lower-than-normal sodium levels in the blood, poses a significant risk, particularly for older adults. According to a study published in the Journal of the American Geriatrics Society, hyponatremia affects up to 7% of the elderly population, with higher rates observed in hospitalized individuals.
As we age, our bodies become less efficient at regulating fluid and electrolyte balance, which increases susceptibility to hyponatremia. Several factors can exacerbate this risk, including underlying medical conditions, medication use, and age-related physiological changes. Early recognition and appropriate management are critical to preventing severe complications and improving outcomes for elderly patients with hyponatremia. How can caregivers effectively recognize subtle indicators of hyponatremia in older adults, and what proactive measures can be implemented to address this potentially serious condition?
Risk Factors for Sodium Deficiency in Seniors
Age-related sodium deficiency; medication-induced hyponatremia; senior health risks; fluid balance
Multiple factors contribute to the increased risk of hyponatremia in older adults. Chronic medical conditions, such as heart failure, kidney disease, and liver cirrhosis, can impair the body’s ability to regulate fluid and electrolyte balance, predisposing individuals to hyponatremia. Certain medications, particularly diuretics, antidepressants (SSRIs), and pain medications, can interfere with sodium regulation and increase the risk of hyponatremia. Age-related physiological changes, such as decreased kidney function, reduced thirst sensation, and hormonal imbalances, can further compromise sodium balance and increase susceptibility to hyponatremia. A study in the Clinical Journal of the American Society of Nephrology found that thiazide diuretics, commonly prescribed, could induce hyponatremia. Understanding these risk factors is essential for identifying individuals at high risk and implementing targeted prevention strategies.
Spotting the Signs: Recognizing Symptoms of Hyponatremia
Hyponatremia symptoms in elderly; recognizing low sodium; neurological symptoms; physical symptoms
Recognizing the symptoms of hyponatremia is crucial for early diagnosis and timely intervention. However, the symptoms can be subtle and nonspecific, often mimicking other age-related conditions. Common symptoms of mild to moderate hyponatremia include:
- Fatigue and weakness
- Nausea and vomiting
- Headache
- Muscle cramps or spasms
- Confusion or disorientation
- Irritability or restlessness
In severe cases, hyponatremia can lead to more serious neurological symptoms, such as seizures, coma, and even death. Given the potential for severe complications, it’s essential to be vigilant for any signs or symptoms of hyponatremia in older adults and seek prompt medical attention if concerns arise. Caregivers should pay close attention to subtle changes in behavior, cognitive function, and physical condition, as these may be early indicators of hyponatremia.
Important Note: It’s impossible to self-diagnose hyponatremia based solely on symptoms. As several medical conditions can cause similar problems, consulting a healthcare professional for accurate diagnosis and treatment is essential.
Diagnosing Low Sodium Levels: Tests and Evaluations
Diagnosing hyponatremia; blood sodium test; urine analysis; diagnostic tools
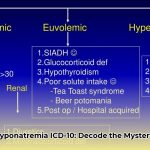
Diagnosing hyponatremia involves a comprehensive evaluation that includes a detailed medical history, physical examination, and laboratory testing. The healthcare provider will inquire about the individual’s medical history, medication use, fluid intake, and any recent symptoms or changes in health status. A physical examination is performed to assess hydration status, neurological function, and overall health. Blood tests are essential for measuring serum sodium levels and assessing kidney function, electrolyte balance, and hormone levels. Urine tests may be conducted to evaluate urine osmolality and sodium concentration, which can help determine the underlying cause of hyponatremia. Imaging tests, such as ultrasound or CT scan, may be necessary to rule out other medical conditions. Accurate diagnosis is crucial for determining the appropriate treatment and management strategies for hyponatremia.
Treatment Strategies: Restoring Sodium Balance Safely
Hyponatremia treatment; restoring sodium levels; medication adjustment; fluid restriction
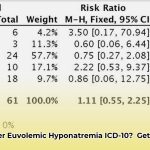
The treatment of hyponatremia focuses on addressing the underlying cause and restoring sodium balance safely and gradually. The specific treatment approach depends on the severity of hyponatremia, the presence of symptoms, and the individual’s overall health status. In mild cases of hyponatremia, treatment may involve restricting fluid intake, adjusting medications, or treating underlying medical conditions. Moderate to severe cases may require intravenous (IV) administration of sodium-containing solutions to gradually increase serum sodium levels. Healthcare providers must closely monitor patients during treatment to prevent rapid overcorrection of hyponatremia, which can lead to serious neurological complications, such as osmotic demyelination syndrome (ODS). According to the National Kidney Foundation, the goal is to correct sodium levels slowly, typically by no more than 8-12 mEq/L in a 24-hour period.
The Role of the Caregiver: Supporting Elderly Patients
Caregiver hyponatremia support; elderly hydration tips; medication management for seniors; monitoring symptoms
Caregivers play a vital role in managing hyponatremia in elderly loved ones. Their responsibilities include:
- Encouraging Hydration: Encourage adequate fluid intake throughout the day, offering water, juice, and other healthy beverages regularly. However, it’s important to balance fluid intake to avoid overhydration, especially in individuals with underlying medical conditions.
- Monitoring Symptoms: Closely monitor for any changes in behavior, cognitive function, or physical condition, such as confusion, nausea, muscle cramps, or seizures. Report any unusual symptoms to the healthcare provider promptly.
- Medication Management: Assist with medication management to ensure adherence to prescribed regimens and monitor for potential side effects. Be particularly vigilant about medications known to affect sodium levels, such as diuretics, antidepressants, and pain medications.
- Promoting a Balanced Diet: Encourage a balanced diet that includes fruits, vegetables, whole grains, and lean protein sources. Limit processed foods high in sodium, as excessive sodium intake can exacerbate fluid retention and electrolyte imbalances.
- Scheduling Regular Check-ups: Ensure regular check-ups with the healthcare provider to monitor sodium levels, assess overall health, and adjust treatment plans as needed. Regular monitoring allows for early detection of hyponatremia and timely intervention to prevent complications.
Potential Symptoms of Hyponatremia: From Mild to Severe
| Symptom Category | Mild Symptoms | Severe Symptoms |
|---|---|---|
| Neurological | Fatigue, headache, mild confusion, drowsiness | Seizures, coma, significant confusion, disorientation |
| Gastrointestinal | Mild nausea | Severe nausea, vomiting, digestive upset |
| Musculoskeletal | Muscle weakness, slight cramps | Severe muscle weakness, cramps, spasms |
| Cardiovascular | Mild lightheadedness, dizziness | Hypotension (low blood pressure), irregular heartbeat |
| Other | Reduced appetite, decreased alertness | Significant appetite loss, lethargy, loss of consciousness |
Promptly seeking medical advice upon noticing these symptoms in an elderly individual is essential. Early detection and intervention can significantly improve the chances of a full recovery.
Safely Correcting Hyponatremia: Gradual and Monitored Approach
Hyponatremia correction; osmotic demyelination syndrome; safe hyponatremia treatment; treatment risks
Key Takeaways:
- Hyponatremia, characterized by low sodium levels, is prevalent among older adults and often presents subtle and easily overlooked symptoms.
- Several factors contribute to hyponatremia in seniors, including medications, dietary factors, age-related physiological changes, and underlying medical conditions.
- Safely correcting hyponatremia in elderly patients necessitates careful monitoring and a gradual approach to prevent potential complications.
- Early detection is crucial, emphasizing the importance of regular checkups and heightened awareness of potential symptoms.
- Collaborating closely with healthcare professionals is essential to develop personalized treatment plans tailored to individual needs and circumstances.
Understanding Hyponatremia: Risk Factors and Causes
Elderly hyponatremia causes; age-related hyponatremia; hyponatremia risk factors; underlying conditions
Hyponatremia poses a significant health risk to older adults, often presenting with nonspecific symptoms easily mistaken for other age-related conditions. Distinguishing
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026