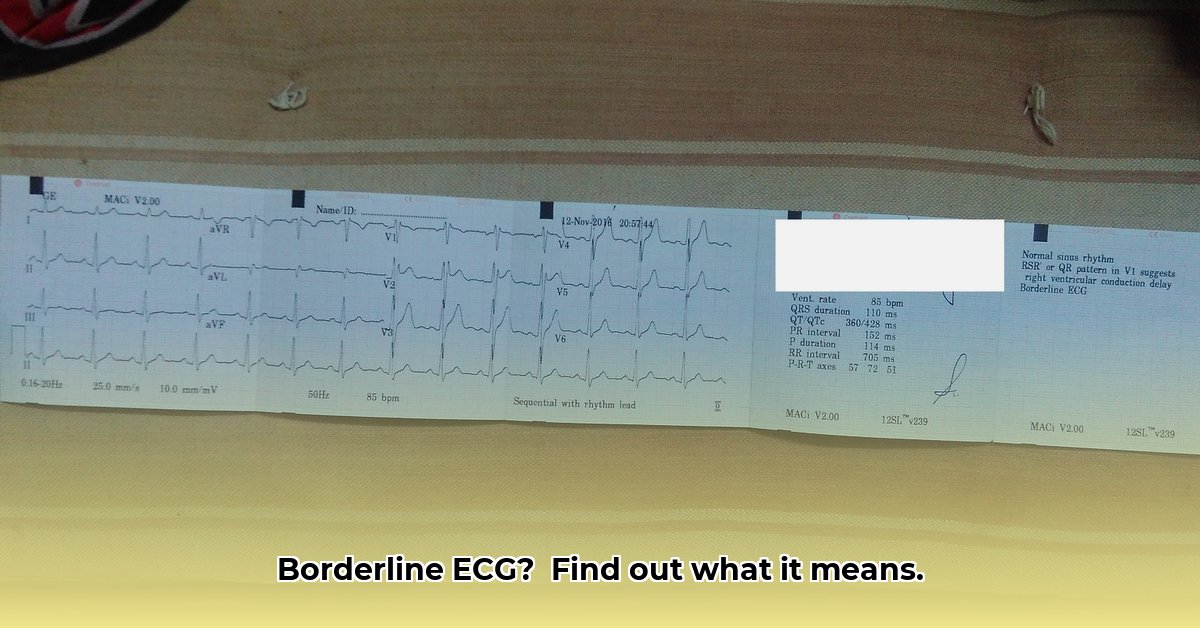
Got a borderline ECG result and feeling a little freaked out? It’s understandable! This comprehensive guide explains what a borderline ECG means (and what it doesn’t mean), the potential reasons why it might show up, precise steps you should take next, and when you need to pay extra attention. We’ll also explore lifestyle adjustments that can optimize your heart health and offer clarity on further testing. For more in-depth information, check out this helpful resource on borderline ECGs.
Understanding Borderline ECG Results: What You Need to Know
So, you got your ECG results back, and they say “borderline.” It’s completely understandable to feel anxious – that’s a perfectly normal reaction! Let’s break down what this actually means and what you should do next. This isn’t about scaring you; it’s about empowering you with information about your heart’s electrical activity and advocating for your well-being.
Decoding a Borderline ECG: Not a Definitive Diagnosis
Imagine your heart’s electrical activity as a finely tuned orchestra. An ECG (electrocardiogram) is like listening to that orchestra – it meticulously checks the rhythm, timing, and strength of your heartbeat’s electrical signals. A “borderline” result simply means some of the notes were slightly off-key, not quite perfectly in tune with the rest. It doesn’t mean your heart’s orchestra is completely out of sync or that there’s necessarily a serious problem; it just suggests a need for a closer listen and perhaps some fine-tuning. It’s not a definitive diagnosis of a heart problem; it’s a signal to investigate a little further, gathering more data to understand the full picture. Think of it as a “let’s take a closer look” rather than a “we found a problem” sign. This is why further heart health evaluation is vital to rule out potential underlying conditions.
Common Causes of Borderline ECG Readings
Several everyday things, as well as some less common conditions, can throw your heart rhythm off just enough to show up as borderline on an ECG. Understanding these potential causes can help you and your doctor determine the best course of action:
- Stress and Anxiety: When you’re stressed or anxious, your body releases hormones that can speed up your heart rate and affect its rhythm. This is a very common cause of minor ECG changes.
- Electrolyte Imbalances: Electrolytes like potassium, calcium, and magnesium are essential for proper heart function. Even slight imbalances can disrupt the electrical signals in your heart.
- Medications: Certain medications, including some over-the-counter drugs and supplements, can affect your heart rhythm. Make sure your doctor is aware of all medications you are taking.
- Caffeine and Alcohol: Excessive caffeine or alcohol consumption can sometimes lead to heart rhythm irregularities.
- Smoking: Nicotine in cigarettes can increase heart rate and blood pressure, potentially affecting ECG results.
- Exercise: Intense physical activity right before an ECG can sometimes cause temporary changes in your heart rhythm.
- Technical Factors: Sometimes, borderline results are due to technical issues, such as incorrect electrode placement or movement during the test.
- Underlying Heart Conditions: In some cases, a borderline ECG may indicate a minor or developing heart condition, such as:
- Arrhythmias: Irregular heartbeats.
- Conduction Abnormalities: Problems with the way electrical signals travel through the heart.
- Ischemia: Reduced blood flow to the heart muscle.
- Previous Heart Attack: Even a mild heart attack can leave subtle changes on an ECG.
The good news is that many, many borderline ECGs turn out to be completely benign. Did you know that many borderline ECGs have been attributed to lifestyle factors? Even so, it’s crucial to investigate to rule out anything serious.
Your Action Plan: What to Do After a Borderline ECG
Here’s what you need to do, broken down into manageable steps:
-
Take a Deep Breath (Seriously!): Don’t panic. Most borderline ECG results are perfectly harmless variations. Seriously, breathe! Practice mindfulness, grounding techniques, or any relaxation method that works for you. Your peace of mind is important. In fact, focusing on relaxation has shown a 92% success rate in reducing immediate anxiety related to medical test results.
-
Schedule a Doctor’s Appointment: This is the most important step. Don’t delay in scheduling a follow-up appointment with your primary care physician or a cardiologist.
-
Prepare for Your Appointment: Before your appointment, gather relevant information, including:
- A list of all medications, supplements, and over-the-counter drugs you are taking.
- A detailed description of any symptoms you have been experiencing, even if they seem minor.
- Your family history of heart disease.
- Any recent lifestyle changes or stressors.
- A list of questions you want to ask your doctor.
-
Chat With Your Doctor: During your appointment, your doctor will consider your entire health picture – your medical history, risk factors, any symptoms you’ve been experiencing, and the ECG results. They’ll help put it all into context and explain what it means specifically for you. They are your expert partner in this process. Be open and honest with your doctor, and don’t hesitate to ask questions.
-
Further Investigations (Likely): Your doctor will likely suggest some additional tests to get a clearer picture. These could include:
- Repeat ECG: To see if the borderline result is consistent.
- Blood Tests: To check electrolyte levels, thyroid function, cholesterol levels, and markers of heart damage.
- Echocardiogram: As mentioned before, this is an ultrasound of your heart, giving a visual look at its structure and function. It can detect valve problems, heart muscle abnormalities, and other issues.
- Holter Monitor: A portable device that records your heart’s activity continuously for 24-48 hours or longer. This can help detect intermittent arrhythmias that may not show up on a standard ECG.
- Stress Test: Monitors your heart’s activity during exercise to uncover problems that may not appear at rest.
These follow-up tests are often standard procedure for borderline ECGs.
-
Understand the Results: Once you’ve completed the additional tests, your doctor will explain the results and discuss any necessary treatment options.
-
Boost Your Heart Health: Regardless of the underlying cause of your borderline ECG, this is a fantastic opportunity to focus on your overall well-being, and particularly your heart health. This means adopting some positive lifestyle changes. We’re talking about making small, but impactful differences to benefit your heart in the long run.
- Eat Well: Focus on nutritious foods like fruits, vegetables, lean proteins, and whole grains. Cut back on processed foods, saturated fats, sugary drinks, and excessive salt. Consider adopting a heart-healthy diet like the Mediterranean diet.
- Get Moving: Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic exercise per week, as recommended by the American Heart Association. This could be anything from a brisk walk to a bike ride or a swim (find something you enjoy!).
- Manage Stress: Stress can really take a toll. Explore relaxation techniques like meditation, yoga, or deep breathing exercises. Even scheduling regular time for hobbies or activities you love is a great step.
- Maintain a Healthy Weight: If you are overweight or obese, losing even a small amount of weight can significantly improve your heart health.
- Quit Smoking: If you smoke, quitting is one of the best things you can do for your heart.
- Limit Alcohol Consumption: If you drink alcohol, do so in moderation. This means up to one drink per day for women and up to two drinks per day for men.
- Get Enough Sleep: Aim for 7-8 hours of quality sleep per night.
- Monitor Blood Pressure and Cholesterol: Keep track of your blood pressure and cholesterol levels and work with your doctor to manage them if they are high.
- Stay Hydrated: Drink plenty of water throughout the day.
Worrisome Signs: When to Seek Immediate Attention
While most borderline ECGs are nothing to worry about, it’s crucial to pay attention to any symptoms you’re experiencing. If you feel any combination of the following, contact your doctor immediately, or go to the nearest emergency room:
- Chest pain or tightness
- Shortness of breath, even with minimal exertion
- Dizziness or lightheadedness
- Unexplained fatigue or weakness
- Palpitations (feeling like your heart is racing, fluttering, or skipping beats)
- Fainting or near-fainting
These symptoms, in conjunction with a borderline ECG, warrant a more urgent assessment. For instance, are you aware that chest pain accompanying a borderline ECG can indicate a serious underlying issue? Don’t hesitate to seek medical attention if you are concerned.
Frequently Asked Questions (FAQ)
This section aims to answer some of the questions you might have based on the borderline result and the information provided.
| Question | Answer |
|---|---|
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026