Kidney failure frequently results in low blood sodium levels, a condition known as renal failure hyponatremia. This significantly impacts patients with chronic kidney disease (CKD) or end-stage renal disease (ESRD). For more detailed ICD-10 codes, see this helpful resource: ICD-10 codes. When kidneys struggle to balance water and salt, the disruption causes various symptoms ranging from headaches and nausea to severe issues like seizures or coma. The severity is directly related to the sodium level and rate of decline. Understanding this condition and employing effective management strategies are crucial for improving patient outcomes.
Understanding Hyponatremia: Causes and Diagnosis
Hyponatremia in renal failure arises from multiple factors. Fluid overload, a consequence of impaired kidney function, leads to excess fluid buildup. This dilutes the blood and reduces sodium concentrations. Diuretics, often prescribed to manage fluid overload, can paradoxically worsen hyponatremia by promoting sodium loss. Underlying conditions such as heart failure, liver disease, and syndrome of inappropriate antidiuretic hormone secretion (SIADH) can further complicate the clinical picture.
Classifying hyponatremia based on fluid volume status helps guide treatment. Hypovolemic hyponatremia involves both sodium and fluid loss, while euvolemic hyponatremia presents with normal fluid volume. Hypervolemic hyponatremia, common in renal failure, is characterized by excess fluid. Identifying the specific type is critical for appropriate intervention.
In addition to fluid status, other critical causes of hyponatremia in CKD patients include:
- Medications: Certain medications, including thiazide diuretics, some antidepressants (SSRIs), and pain medications, can contribute to hyponatremia.
- Hormonal Imbalances: Conditions affecting hormone production, such as hypothyroidism and adrenal insufficiency, can disrupt sodium balance.
- Dietary Factors: While less common, insufficient sodium intake can, in rare cases, contribute to hyponatremia, especially in individuals with significant sodium losses.
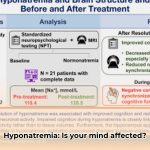
Diagnosis begins with a blood test measuring serum sodium levels. A level below 135 mEq/L indicates hyponatremia. Further investigations include assessing kidney function (glomerular filtration rate, urine output), electrolyte balance (potassium, chloride, bicarbonate), and osmolality (both serum and urine). A thorough medical history, including medication review and assessment for underlying conditions, is essential.
Treatment Strategies: A Personalized Approach
Treatment for renal failure hyponatremia aims to address the underlying cause and restore normal sodium levels gradually. The approach varies depending on the severity of hyponatremia, the patient’s fluid status, and the presence of other medical conditions.
- Fluid Restriction: In hypervolemic hyponatremia, limiting fluid intake helps reduce dilution and raise sodium levels.
- Diuretic Adjustment: Careful adjustment of diuretic doses is crucial, balancing fluid management with the risk of further sodium loss.
- Sodium Supplementation: In some cases, oral or intravenous sodium supplementation may be necessary to correct severe hyponatremia. This must be done cautiously to avoid overcorrection.
- Medications: In specific situations, medications like vasopressin receptor antagonists (vaptans) may be considered to promote water excretion without sodium loss. However, these medications require careful monitoring due to potential side effects.
The rate of sodium correction is critical. Rapid correction can lead to osmotic demyelination syndrome (ODS), a potentially devastating neurological complication. The target rate of correction is typically no more than 4-6 mEq/L per 24 hours.
Hyponatremia Management in Dialysis Patients
For patients undergoing dialysis, managing hyponatremia presents unique challenges. Dialysis itself can influence sodium levels, requiring careful monitoring and adjustments to the dialysis prescription. Strategies include:
- Dialysate Sodium Concentration: Adjusting the sodium concentration of the dialysate fluid can help correct hyponatremia during dialysis.
- Ultrafiltration Rate: Controlling the rate of fluid removal (ultrafiltration) during dialysis can help manage fluid balance and sodium levels.
- Frequent Monitoring: Regular monitoring of serum sodium levels before, during, and after dialysis is essential to guide treatment.
“Careful management of fluid balance and sodium levels during dialysis is crucial in preventing and treating hyponatremia,” explains [Dr. Michael Choi, Professor of Medicine, Division of Nephrology, Johns Hopkins University School of Medicine].
Dietary Considerations
While low-sodium diets are generally recommended for patients with kidney disease to manage blood pressure and fluid retention, the optimal sodium intake for patients with renal failure hyponatremia is debated. Excessive sodium restriction can sometimes worsen hyponatremia.
A collaborative approach involving a nephrologist and a registered dietitian is essential to determine the appropriate sodium intake for each patient, balancing the need to manage fluid overload with the risk of exacerbating hyponatremia. The dietary plan should also ensure adequate intake of other essential nutrients.
Collaborative Care: A Multidisciplinary Approach
Effective management of renal failure hyponatremia requires a collaborative effort among nephrologists, primary care physicians, nurses, dietitians, and pharmacists. Regular communication, shared decision-making, and coordinated care plans are vital for optimizing patient outcomes.
Special Considerations
Assessing Risk Factors
Identifying patients at high risk for hyponatremia is a key step in proactive management. Risk factors include:
| Risk Level | Patient Characteristics | Management |
|---|---|---|
| High | Very low sodium (<120 mEq/L), rapid onset, significant symptoms, underlying conditions | Immediate medical attention, close monitoring, intravenous sodium correction (cautiously), investigation of underlying causes |
| Moderate | Mild to moderately low sodium, multiple electrolyte imbalances, diuretic use | Frequent monitoring, adjustment of medications, fluid restriction, dietary evaluation, consideration of underlying conditions |
| Low | Mild, slowly developing low sodium, few symptoms, stable condition | Regular monitoring, education on fluid intake, review of medications, dietary assessment, consideration of underlying conditions |
Hyponatremia Management in Elderly CKD Patients with Heart Failure
Elderly patients with CKD and heart failure are especially vulnerable to hyponatremia due to age-related physiological changes, multiple comorbidities, and polypharmacy. Management requires a highly individualized approach, considering the complex interplay of these factors.
Accurate diagnosis is essential to distinguish between hypervolemic and hypovolemic hyponatremia. Treatment strategies include fluid restriction, careful diuretic management, and medication review. Close monitoring and proactive management of comorbidities are crucial for preventing complications.
Hypervolemic Hyponatremia in Dialysis Patients
Hypervolemia combined with hyponatremia in dialysis patients poses significant treatment challenges. The goal is to simultaneously manage fluid overload and correct hyponatremia while minimizing the risk of ODS.
Strategies include fluid restriction, dietary sodium management, adjusted ultrafiltration during dialysis, and, in some cases, continuous venovenous hemofiltration (CVVH). Close monitoring of serum sodium levels and fluid status is essential throughout treatment.
Future Research and Patient Empowerment
Ongoing research is focused on refining treatment strategies for renal failure hyponatremia, identifying novel therapeutic targets, and developing personalized approaches tailored to individual patient needs. Areas of investigation include:
- Predictive models for hyponatremia risk
- The impact of different dialysis modalities on sodium balance
- The role of novel biomarkers in guiding treatment
- Long-term outcomes of different treatment strategies
Patient education plays a vital role in long-term management. Empowering patients to understand the risks of hyponatremia, recognize symptoms, adhere to treatment plans, and communicate effectively with their healthcare team can significantly improve outcomes and quality of life.
Disclaimer: This information is intended for educational purposes only and does not constitute medical advice. Always consult with your physician or nephrologist for diagnosis and treatment of hyponatremia.
- How Much Do Wellness Programs Cost Businesses To Offer? - December 16, 2025
- Wellness Fair Ideas for Work to Boost Employee Wellbeing - December 15, 2025
- Affordable Employee Wellness Fair Ideas for Any Budget - December 14, 2025