Hyponatremia, defined by a serum sodium concentration below 135 mmol/L, represents a frequently encountered yet multifaceted clinical challenge. Effective management demands an evidence-based approach, focusing on individualized treatment strategies to avert complications such as cerebral edema and osmotic demyelination syndrome (ODS). For more detailed guidelines, see this comprehensive resource. Failure to address hyponatremia promptly and accurately can lead to significant morbidity and mortality, underscoring the importance of an informed, evidence-driven approach for clinicians.
Diagnosing and Classifying Hyponatremia: A Comprehensive Guide to Sodium Imbalance
The cornerstone of effective hyponatremia management lies in accurate and timely diagnosis. A systematic approach, incorporating clinical assessment and laboratory investigations, is crucial to identify the underlying etiology and guide appropriate treatment.
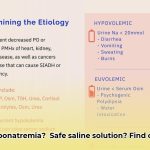
- Assess Volume Status: Categorize hyponatremia based on extracellular fluid volume status: hypovolemic, euvolemic, or hypervolemic. Clinical signs such as orthostatic hypotension, tachycardia, and edema can aid in this determination.
- Evaluate Serum Osmolality: Measure serum osmolality to confirm true hyponatremia (hypotonic hyponatremia) and rule out pseudohyponatremia or hypertonic hyponatremia.
- Measure Urine Sodium: Urine sodium concentration helps differentiate between renal and extrarenal causes of hyponatremia.
- Consider Medications: Review the patient’s medication list, as many drugs, including diuretics, SSRIs, and certain anti-epileptics, can induce hyponatremia.
- Assess for Underlying Conditions: Evaluate for conditions known to cause hyponatremia, such as SIADH, adrenal insufficiency, hypothyroidism, heart failure, and liver cirrhosis.
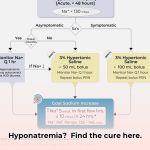
Acute vs. Chronic Hyponatremia
Distinguishing between acute (onset < 48 hours) and chronic (onset > 48 hours) hyponatremia is crucial, as it dictates the urgency and approach to treatment. Acute hyponatremia carries a higher risk of cerebral edema, while chronic hyponatremia poses a greater risk of ODS with rapid correction.
Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH)
SIADH is a common cause of euvolemic hyponatremia, characterized by excessive ADH release despite low serum osmolality. Diagnosis requires excluding other causes of euvolemic hyponatremia, such as adrenal insufficiency and hypothyroidism.
Diagnostic Criteria for SIADH:
- Hypotonic hyponatremia (serum sodium < 135 mmol/L)
- Low serum osmolality (< 275 mOsm/kg)
- Elevated urine osmolality (> 100 mOsm/kg)
- Urine sodium > 40 mmol/L with normal salt and water intake
- Euvolemia
- Exclusion of adrenal insufficiency, hypothyroidism, and renal disease
Treatment Strategies: Tailoring Interventions for Optimal Outcomes
Managing hyponatremia requires a nuanced, individualized approach, with the primary goal of correcting serum sodium levels gradually and safely while addressing the underlying cause.
- Fluid Restriction: A cornerstone of treatment for euvolemic and hypervolemic hyponatremia, particularly in SIADH. Limiting fluid intake to 500-1000 mL/day can promote negative water balance and increase serum sodium.
- Sodium Correction: The rate of sodium correction is paramount to prevent neurological complications. The recommended rate is no more than 6-8 mmol/L per 24 hours, with a target of 4-6 mmol/L in the first 24 hours for chronic hyponatremia.
- Hypertonic Saline: Reserved for severe, symptomatic hyponatremia (e.g., seizures, coma) or acute hyponatremia with rapid decline in serum sodium. Administer hypertonic saline (3% NaCl) cautiously, with frequent monitoring of serum sodium levels.
- Vaptans (Vasopressin Receptor Antagonists): Vaptans, such as tolvaptan and conivaptan, block the action of ADH in the kidneys, promoting water excretion and increasing serum sodium. They are useful for euvolemic and hypervolemic hyponatremia, particularly in SIADH and heart failure.
- Loop Diuretics: In hypervolemic hyponatremia, loop diuretics (e.g., furosemide) can promote sodium and water excretion, improving serum sodium levels.
- Treat Underlying Cause: Addressing the underlying cause of hyponatremia is essential for long-term management. This may involve discontinuing offending medications, treating adrenal insufficiency or hypothyroidism, or managing heart failure.
Risk Assessment Matrix: Weighing Treatment Options
| Treatment | Risk of Cerebral Edema | Risk of ODS | Risk of Overcorrection | Monitoring Frequency | Indications |
|---|---|---|---|---|---|
| Fluid Restriction | Low | Low | Low | Regular | Euvolemic/Hypervolemic Hyponatremia, SIADH |
| Cautious Sodium Correction | Low | Low | Low | Frequent | Chronic Hyponatremia |
| Hypertonic Saline | Moderate | Low | High | Very Frequent | Severe/Symptomatic Hyponatremia, Acute Hyponatremia |
| Vaptans | Low | Low | Moderate | Frequent | Euvolemic/Hypervolemic Hyponatremia, SIADH, Heart Failure |
| Loop Diuretics | Low | Low | Low | Frequent | Hypervolemic Hyponatremia |
How to Safely Manage Hyponatremia in High-Risk Patients
Close monitoring is paramount when managing hyponatremia, especially in high-risk patients.
- Frequent Monitoring: Monitor serum sodium levels every 4-6 hours during active correction, and adjust treatment accordingly.
- Neurological Assessments: Regularly assess for neurological changes, such as confusion, lethargy, seizures, or changes in mental status, which may indicate cerebral edema or ODS.
- Individualized Approach: Tailor treatment to the patient’s age, medical history, and severity of hyponatremia.
- Avoid Overcorrection: Adhere to the recommended correction rate of 6-8 mmol/L per 24 hours to minimize the risk of ODS.
- Consider Comorbidities: Account for underlying conditions, such as kidney disease, liver disease, and heart failure, which can affect sodium and water balance.
Understanding Hyponatremia in Specific Patient Populations
Specific patient populations require tailored management strategies.
- Elderly Patients: Elderly individuals are more susceptible to hyponatremia due to age-related changes in renal function and increased prevalence of comorbidities. They may also present with atypical symptoms, making diagnosis challenging.
- Heart Failure Patients: Hyponatremia is common in heart failure and is associated with increased mortality. Management involves fluid restriction, loop diuretics, and, in some cases, vaptans.
- Cirrhosis Patients: Liver cirrhosis can lead to hyponatremia due to impaired water excretion and increased ADH levels. Management includes fluid restriction, sodium restriction, and, in refractory cases, vaptans or liver transplantation.
Advanced Hyponatremia Management: Addressing Rare Subtypes and Co-morbidities
In complex cases of hyponatremia, it’s crucial to consider rare subtypes and co-morbidities.
- Drug-Induced Hyponatremia: Certain medications, such as psychotropic drugs, can induce hyponatremia through SIADH or other mechanisms. Discontinuing or adjusting the dose of the offending medication may be necessary.
- Cerebral Salt Wasting (CSW): CSW is a rare condition characterized by hyponatremia and hypovolemia due to excessive sodium excretion by the kidneys. Management involves sodium and fluid replacement.
- Nephrogenic Syndrome of Inappropriate Antidiuresis (NSIAD): NSIAD is a rare genetic disorder caused by gain-of-function mutations in the V2 vasopressin receptor gene, leading to constitutive activation of the receptor and water retention. Management involves fluid restriction and vaptans.
Expert Insight:
“A collaborative approach involving nephrologists, endocrinologists, and other specialists is crucial for managing advanced hyponatremia cases,” emphasizes Dr. [Full Name and Title], [Position] at [Institution]. This multidisciplinary strategy ensures that both the electrolyte imbalance and underlying medical conditions are addressed comprehensively.
Actionable Steps:
- Thoroughly evaluate medication lists to identify potential drug-induced causes of hyponatremia.
- Consider rare conditions like CSW or NSIAD in patients with unexplained hyponatremia.
- Involve a multidisciplinary team to optimize management of complex hyponatremia cases.
Future Directions:
Ongoing research aims to refine hyponatremia management strategies and improve patient outcomes.
- Biomarkers for ODS: Development of biomarkers for early detection of ODS would allow for timely intervention and prevention of permanent neurological damage.
- Personalized Treatment Approaches: Future studies should focus on identifying patient-specific factors that predict response to different treatments, allowing for more personalized management strategies.
- Novel Therapies: Research is ongoing to develop novel therapies that target the
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026