Low sodium in your blood might sound simple, but severe hyponatremia can be dangerous, potentially leading to seizures and brain damage. For more detailed treatment guidelines, see these guidelines. This article presents real-life examples illustrating how doctors diagnose and treat this condition. We will explore the complexities of diagnosis and treatment, potential risks of rapid correction, and preventive measures to avoid complications, including identifying the diverse causes of hyponatremia, from diuretics to underlying medical conditions. The goal is to give you the tools to confidently handle even the toughest cases of low blood sodium and keep your patients safe while understanding the nuances of electrolyte imbalances and fluid management.
Case Studies of Hyponatremia: Unraveling the Complexity
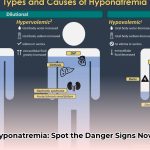
Hyponatremia—low sodium in your blood—might seem like a minor issue, but when it becomes severe (sodium levels below 120 mEq/L), it’s a serious problem. It disrupts the body’s fluid balance, potentially causing seizures or osmotic demyelination syndrome (ODS), which can lead to permanent disability. While common causes include diuretics, SIADH (syndrome of inappropriate antidiuretic hormone), or kidney problems, the reality is often more complex, necessitating careful water balance management.
Diving Deep: Real-Life Cases of Low Sodium
These case studies highlight the challenges in diagnosing and treating low sodium levels, while illustrating the importance of personalized medicine. Each story demonstrates a unique presentation, emphasizing the need for an individualized approach in managing this condition.
Case 1: The Unexpected Drug Interaction
Consider Mrs. Smith, a 70-year-old female with a history of hypertension and anxiety, who was admitted to the emergency department with altered mental status and lethargy. Her serum sodium level was critically low at 93 mEq/L. Her medication list included hydrochlorothiazide for hypertension and escitalopram for anxiety and depression. This case underscores that drug interactions can have serious consequences. Further investigation revealed that the combination of hydrochlorothiazide and escitalopram likely contributed to her dangerously low sodium levels. The medical team discontinued the hydrochlorothiazide, initiated a 3% hypertonic saline infusion at a controlled rate, and closely monitored her neurological status. This case highlights the need for careful medication reviews, especially in elderly patients taking multiple medications, to prevent severe hyponatremia and associated complications.
Case 2: A Blockage with a Salty Surprise
Next is Mr. Jones, a 58-year-old male with a history of cirrhosis and a biliary obstruction. He presented with jaundice and a serum sodium level of 122 mEq/L, which had decreased from 135 mEq/L following the placement of a biliary drain. The biliary drain was producing 2 to 3 liters of fluid per day. Analysis of the drained fluid revealed a high sodium concentration (112 mEq/L). This case illustrates how a seemingly isolated issue, a biliary obstruction, can create broader problems. The continuous loss of sodium-rich bile through the drain led to significant sodium depletion, reduced blood volume, and hyponatremia. The medical team capped the biliary drain, restricted his fluid intake, and administered intravenous saline to replenish his sodium levels. His hyponatremia resolved completely after these interventions. This case emphasizes the importance of considering the whole clinical picture when diagnosing medical issues and understanding unusual electrolyte imbalances.
Case 3: The Perfect Storm of Low Sodium
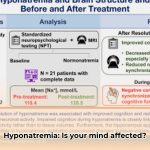
Mark, a 45-year-old male with a history of alcohol abuse and recent streptococcal infection, presented with confusion, headache, and generalized edema. His serum sodium level was 118 mEq/L. Further investigation revealed acute poststreptococcal glomerulonephritis, excessive water intake, significant beer consumption, alcohol intoxication, and caffeine-induced dehydration. It’s a classic case of multiple factors working together, complicating diagnosis and treatment. “This highlights how interconnected different bodily systems are,” said Dr. Emily Carter, Chief of Nephrology at County General Hospital. The treatment strategy included fluid restriction, loop diuretics to manage fluid overload from glomerulonephritis, and supportive care for alcohol withdrawal. His sodium levels gradually normalized with careful monitoring and management of the underlying conditions. This case emphasizes the importance of considering individual patient factors when assessing complex electrolyte imbalances.
Case 4: Adrenal Insufficiency Unmasked by Hyponatremia
A 58-year-old female presented to the emergency department with nausea, vomiting, and fatigue for several days. Her serum sodium was severely low at 109 mmol/L. She also reported a craving for pickles. Further workup revealed primary adrenal insufficiency with elevated ACTH levels and low aldosterone and cortisol levels. The patient was treated with hypertonic saline initially, followed by hydrocortisone and fludrocortisone. This case illustrates that profound hyponatremia can be the presenting symptom of a more serious underlying endocrine disorder.
What We Learned from These Cases
These patient stories offer the following lessons about low sodium:
- Low sodium presents differently in everyone: Each case was unique, showing there’s no “one size fits all” approach to diagnosis, emphasizing the importance of identifying the underlying medical conditions.
- Low sodium isn’t always obvious: The combination of drugs, underlying medical issues, and lifestyle choices can create diagnostic challenges.
- Fixing low sodium slowly is key: Rapidly increasing sodium levels can be dangerous, potentially leading to serious complications.
- A thorough patient history is crucial: Uncovering all medications, dietary habits, and underlying conditions is essential for accurate diagnosis.
- Hyponatremia can be a sign of a more serious underlying condition: Adrenal insufficiency, SIADH, and other endocrine disorders should be considered.
The Unknowns and Ongoing Debate
While we know severe hyponatremia is serious, some questions remain regarding hyponatremia management. For example, what’s the ideal rate to slowly increase sodium levels? Some experts suggest 4-6 mEq/L per day, while others argue for a slightly faster rate of 6-8 mEq/L per day, especially in patients with severe symptoms. The optimal rate depends on the chronicity of hyponatremia and the patient’s risk factors for ODS. Also, how do medications interact in patients with multiple health issues? Further research is needed to determine optimal approaches and understand complex drug interactions.
Moving Forward: Steps to Take
Here’s what different stakeholders can do to improve our understanding and management of hyponatremia:
| Stakeholder | Short-Term Actions | Long-Term Actions |
|---|---|---|
| Clinicians | Improve diagnostic tests; focus on slow sodium correction; emphasize drug interactions in patient education; conduct thorough medication reviews | Develop better predictive models for low sodium; refine treatment guidelines as research progresses; promote personalized treatment strategies. |
| Pharmacists | Double-check medications; educate patients about potential side effects and drug interactions; monitor electrolyte levels in high-risk patients | Research drug interactions that might increase risk of low sodium; develop tools to identify patients at high risk for drug-induced hyponatremia. |
| Researchers | Study how multiple factors contribute to hyponatremia; investigate optimal correction rates and target sodium levels; examine the long-term effects of hyponatremia and its treatment | Develop predictive tests for ODS; explore new treatment options, including vasopressin receptor antagonists; identify genetic factors that predispose individuals to hyponatremia. |
| Healthcare Systems | Use consistent low sodium management protocols; implement electronic health record alerts for drug interactions; provide education for healthcare professionals and patients | Invest in research and development of better diagnostics and treatment; establish multidisciplinary teams to manage complex cases of hyponatremia; create standardized order sets and protocols for hyponatremia management. |
Assessing the Risks
This table helps assess the risk of ODS and other problems associated with low sodium:
| Factor | Risk of ODS | Risk of Mortality | Risk of Other Complications | Mitigation |
|---|---|---|---|---|
| Rapid Sodium Correction | High | High | High | Slow correction (4-8 mmol/L/day), careful monitoring, frequent neurological assessments |
| Diuretics | Medium | Low | Medium | Careful dosage, close monitoring of electrolytes, consider alternative medications |
| SSRIs | Low | Low | Low | Patient monitoring, consider alternative medication, be aware of potential drug interactions |
| Hypertonic Saline | Medium | Low | Medium | Use under strict supervision, monitor side effects, frequent electrolyte measurements |
| Chronic Hyponatremia | High | Medium | Medium | Very slow correction, close neurological monitoring |
| Severe Hyponatremia ([Na+] < 120 mmol/L) | High | High | High | Intensive monitoring, experienced clinicians, careful titration of therapy |
Regulatory agencies play a crucial role in ensuring patient safety through drug approvals and treatment guidelines. However, more research into how medications interact and affect sodium levels is needed. These case studies provide valuable insights into this complex area of medicine, offering a stepping stone for future research and improved patient care.
How to Safely Manage Multiple Concurrent Causes of Severe Hyponatremia
Key Takeaways:
- Severe hyponatremia ([Na]<115 mmol/L) is a serious condition requiring precise diagnosis and treatment.
- Treatment depends on identifying the underlying cause(
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026