Accurate hyponatremia coding is essential for hospitals to receive proper reimbursement. This guide provides a comprehensive overview of coding hyponatremia cases, avoiding common pitfalls and ensuring correct billing. We’ll explore differentiating hyponatremia types, the influence of comorbidities, and strategies for obtaining necessary information from physicians. Through real-world examples, you’ll gain confidence in coding these cases, supporting both optimal patient care and appropriate hospital reimbursement.
Cracking the Code: Hyponatremia Billing Strategies for Medical Coders
Hyponatremia, or low blood sodium, presents unique challenges for medical coders. Correct billing hinges on understanding the condition’s severity and underlying cause. It’s not solely about a low sodium reading; the complete clinical picture is essential. What treatments were administered? What symptoms were present? These details are paramount for selecting accurate ICD-10 codes, directly influencing reimbursement. Why is pinpointing the specificity of hyponatremia essential for compliant medical billing, and what are the potential consequences of inaccurate coding?
Distinguishing Hyponatremia Subtypes for Precise Coding
Hyponatremia is not a singular condition; various subtypes exist, and distinguishing them is crucial for accurate coding. Consider these scenarios: a dehydrated patient, a fluid-overloaded patient, and one with a different underlying issue. Each situation necessitates a distinct medical approach and potentially different codes. This differentiation is key to precise medical coding. What specific diagnostic criteria and clinical indicators can medical coders use to accurately differentiate between hyponatremia subtypes during the coding process?
While E87.1 is a frequently used primary code, additional codes are often required to reflect associated comorbidities. For instance, many hyponatremia patients also have chronic kidney disease (CKD). Including the appropriate CKD code provides a more comprehensive view of the patient’s overall health, supporting accurate reimbursement.
“Pseudo-hyponatremia” presents a unique challenge. This condition isn’t true low sodium but a falsely low lab result due to elevated blood glucose (hyperglycemia). It’s a deceptive reading that requires careful review of lab results alongside the patient’s symptoms to prevent miscoding. How can medical coders effectively differentiate pseudo-hyponatremia from true hyponatremia when reviewing a patient’s medical chart, and what specific documentation should they look for?
Navigating Active Intervention for Accurate Treatment and Billing Codes
The term “active intervention” is frequently encountered in hyponatremia claims, but its definition can be ambiguous. Some interpret it as any specific treatment, even with minimal symptoms, while others believe significant symptoms are necessary. This lack of standardization necessitates clear internal guidelines and ongoing coder education to ensure consistent application.
What qualifies as “active intervention”? Examples include meticulous fluid management, specific medications like vasopressin receptor antagonists, or other treatments aimed at restoring sodium balance. Thoroughly review medical records for detailed documentation of these interventions. What specific documentation elements should a medical coder prioritize when assessing whether “active intervention” has occurred in a patient’s chart, particularly when the definition seems ambiguous?
Step-by-Step Coding: Leveraging Medical Records
A patient’s medical records are a coder’s most valuable asset. Pay close attention to these crucial details:
- Sodium Levels: Document the frequency of sodium level testing and the corresponding results. Note any patterns of consistently low readings.
- Symptoms: Identify symptoms such as nausea, confusion, seizures, or other neurological indicators. The Glasgow Coma Scale (GCS) score may be included in the record.
- Treatments: Document all treatments administered to address the low sodium, including IV fluids, medications, or other specific interventions.
- Comorbidities: Identify any coexisting conditions that may influence coding, such as CKD, SIADH (Syndrome of Inappropriate Antidiuretic Hormone Secretion), or hyperglycemia. Is it more important to focus on the primary diagnosis or comorbidities that might affect coding accuracy?
If the medical record lacks necessary information, proactively seek clarification from the physician to ensure complete and accurate coding.
Practical Coding Scenarios: Learning from Real-World Examples
Let’s examine practical examples to illustrate key coding principles:
Scenario 1: A patient presents with multiple low sodium readings and severe neurological symptoms such as seizures. They receive IV fluids and medication to elevate their sodium levels. This scenario warrants codes for hyponatremia with complications, along with specific codes for the treatments administered.
Scenario 2: A patient with elevated blood sugar exhibits a single low sodium reading but presents with no symptoms or active treatment. In this situation, assigning the primary hyponatremia code (E87.1) may be inappropriate. Prioritize the overall clinical picture rather than relying solely on a single lab value.
Clinical Situations and ICD-10 Codes: A Quick Reference
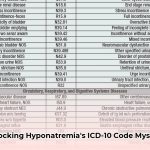
This table provides a summary of how different clinical situations may be coded. Remember that this is a general guide, and individual cases may vary.
| Clinical Picture | Possible ICD-10 Code(s) | Essential Documentation |
|---|---|---|
| Hyponatremia with neurological symptoms | E87.1, G93.4 (and additional codes depending on specifics) | Multiple low sodium levels, neurological indicators, treatments administered |
| Hyponatremia associated with CKD | E87.1, N18. (specify CKD stage) | CKD diagnosis, low sodium levels, specific treatments |
| Pseudo-hyponatremia (secondary to hyperglycemia) | E87.0, E11. (specify type) | Elevated blood sugar, low sodium levels explained by high glucose |
Final Thoughts: Mastering Hyponatremia Medical Coding
This guide serves as a starting point; continuous learning and staying current with the latest coding guidelines are essential for maintaining coding accuracy. Remember that thorough documentation review and careful attention to the clinical picture are the cornerstones of successful and compliant hyponatremia medical coding. Given the evolving nature of medical coding standards and ongoing research in this area, what are the most reliable and current resources for staying updated on hyponatremia coding practices?
Accurate Hyponatremia Coding in the Presence of Multiple Comorbidities
Key Takeaways:
- Accurate hyponatremia coding depends on detailed clinical documentation demonstrating active medical intervention. Documenting only low sodium levels is insufficient.
- Coding hyponatremia with multiple comorbidities necessitates the use of both primary (E87.1) and secondary ICD-10 codes to reflect all diagnoses.
- Differentiate between true hyponatremia and pseudo-hyponatremia (caused by hyperglycemia).
- Thoroughly understand hyponatremia subtypes (hypovolemic, euvolemic, hypervolemic) for accurate coding.
- Comprehensive documentation, including the Glasgow Coma Scale (GCS) score where relevant, supports accurate billing and prevents claim denials.
Hyponatremia and Comorbidities: Understanding the Complexity
Hyponatremia, characterized by abnormally low sodium levels in the blood, presents a considerable coding challenge. It is rarely a standalone diagnosis; comorbidities frequently complicate the clinical picture. You must know how to accurately code hyponatremia with multiple comorbidities. Why? Incomplete coding can lead to claim denials and revenue loss, negatively impacting healthcare organizations.
Essential Elements for Accurate Hyponatremia Coding
Coding goes beyond simply identifying low sodium. Effective coding requires evidence of active medical intervention. What defines “active intervention”? It’s more than mere monitoring; it involves active treatment, such as fluid management or medication adjustments. Your documentation must explicitly detail these interventions.
- Multiple Sodium Readings: Document at least two instances of low sodium levels. The specific number of readings needed may vary depending on the clinical context and presentation.
- Clinical Symptoms: Provide thorough documentation of the patient’s symptoms. These symptoms provide critical context for the diagnosis and the necessity for intervention.
- Treatment Plan: Clearly outline the physician’s treatment strategy, specifying the types of fluids administered, medication adjustments performed, and the patient’s response to the interventions.
- Comorbidities: Accurately identifying and coding all associated conditions is essential for complete reimbursement. Examples include congestive heart failure (CHF), chronic kidney disease (CKD), and syndrome of inappropriate antidiuretic hormone secretion (SIADH). Assign appropriate secondary codes to reflect these conditions.
Hyponatremia Subtypes: Guiding Your Coding Decisions
Hyponatremia is not a single entity; it comprises three main subtypes: hypovolemic, euvolemic, and hypervolemic. Each subtype necessitates a nuanced coding approach that accurately reflects the underlying cause. Understanding these distinctions is crucial when coding hyponatremia with multiple comorbidities.
- Hypovolemic Hyponatremia: This subtype, characterized by fluid loss, necessitates documenting the cause of the fluid loss (e.g., vomiting, diarrhea, diuretic use).
- Euvolemic Hyponatremia: In euvolemic hyponatremia, the total body water increases with normal sodium levels, as seen in SIADH. Document the underlying cause – SIADH, medication-induced, etc.
- Hypervolemic Hyponatremia: Here, both sodium and water increase, but water excess is greater. Common causes include heart failure, liver disease, and kidney failure. Accurately coding the underlying condition is vital.
- How Much Do Wellness Programs Cost Businesses To Offer? - December 16, 2025
- Wellness Fair Ideas for Work to Boost Employee Wellbeing - December 15, 2025
- Affordable Employee Wellness Fair Ideas for Any Budget - December 14, 2025