Getting a “borderline” result on your EKG can be worrying, especially if heart disease runs in your family. It doesn’t mean you definitely have a problem, but it does mean your doctor wants to take a closer look. For more information on further testing, see this helpful guide on borderline EKG testing. This article will explain what a borderline EKG means in plain English, how your family history matters, and what steps you should take next. We’ll break down the information clearly, so you can understand your results and feel confident about your next steps to better heart health. Let’s figure this out together.
Borderline ECG: Decoding Heart Health Risks and Family Ties
Let’s talk about something that might sound a little scary: a borderline ECG reading and a family history of heart problems. But before you panic, let’s break it down in a way that’s easy to understand. This isn’t about fear; it’s about empowering you with knowledge to take charge of your heart health.
What’s a Borderline ECG, Anyway? Understanding Electrical Activity
Imagine your heart’s electrical activity as a report card. An electrocardiogram (ECG) – also known as EKG – is like looking at that report card. A “borderline” ECG isn’t a failing grade; it’s more like a “needs improvement.” Something’s slightly off, something the doctor wants to look at more closely. It’s not necessarily a sign of a major problem, but it’s a signal to learn more. This is especially important if heart disease runs in your family.
Think of it like a yellow traffic light – it’s not a full stop, but it’s definitely a warning to slow down and proceed with caution. It’s a prompt to take some extra steps to understand what’s happening with your heart.
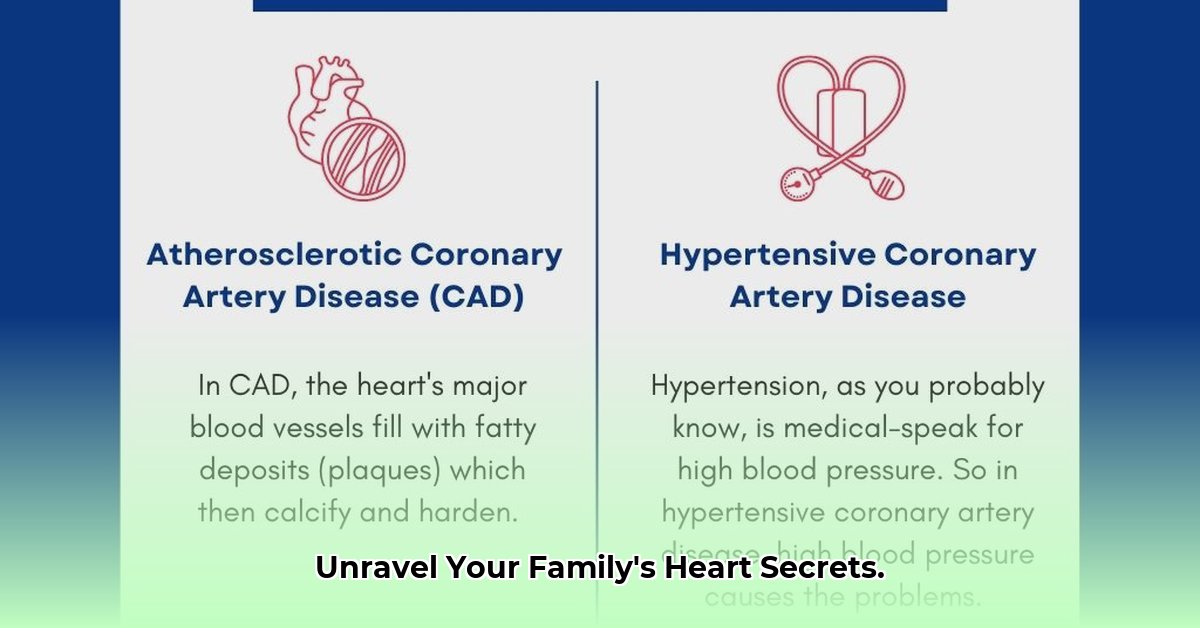
Family History: Genes and Increased Risk
Genetics play a significant role in our health. If your parents, grandparents, aunts, uncles, or siblings have had heart attacks, strokes, irregular heartbeats (arrhythmias), or other heart issues, you’re statistically more likely to experience similar problems. It doesn’t guarantee you’ll develop heart disease, but it increases your chances. Knowing your family’s history is crucial for preventative care.
This isn’t about dwelling on the negative; it’s about being proactive. Understanding your family’s health history empowers you to make smart choices about your health. Don’t underestimate the power of knowing your risk factors.
A Borderline ECG and Family History: Your Action Plan
If you have both a borderline ECG and a family history of heart disease, don’t panic, but do take action! Here’s a step-by-step guide:
-
Talk to Your Doctor (Seriously!): This is the most important step. Schedule an appointment and discuss your ECG results and family medical history in detail. Your doctor is your best resource for understanding what your results mean and what steps you should take next.
-
Prepare for More Tests (Likely): Your doctor might recommend additional tests to get a clearer picture of your heart’s health. This could include blood tests to check cholesterol levels, a stress test to see how your heart responds to exercise, or even an echocardiogram. Don’t be afraid to ask questions about these tests; understanding the process will help ease any anxiety.
-
Lifestyle Tweaks (Always a Good Idea): Regardless of the results of other tests, making heart-healthy lifestyle changes is always beneficial. This is about giving your heart the best chance it can get. This includes, but is not limited to:
- Regular Exercise: Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic activity per week.
- Balanced Diet: Focus on fruits, vegetables, whole grains, and lean proteins. Limit saturated and trans fats, sodium, and sugary drinks. Small changes can make a big difference.
- Stress Management: Find healthy ways to manage stress. This could include yoga, meditation, spending time in nature, or simply taking some time for yourself each day.
- Quit Smoking (If Applicable): Smoking significantly increases your risk of heart disease. If you smoke, quitting is one of the best things you can do for your heart health. Your doctor can help you find resources to quit.
-
Follow Up & Stay Connected: Consistent follow-up appointments with your doctor are key. Don’t hesitate to contact your doctor between appointments if you have any questions or concerns. Staying connected to your healthcare team ensures ongoing monitoring and support.
Understanding the Bigger Picture: Proactive Prevention
A borderline ECG might just mean a temporary issue, such as stress, dehydration, or an electrolyte imbalance. But, coupled with a family history of heart disease, it raises the possibility of underlying conditions that require attention. It’s about proactive prevention, not just reactive treatment.
Working Together for Your Heart Health: Communicating With Your Healthcare Team
Remember, you’re not alone. Your doctor and healthcare team are there to support you every step of the way. Open communication is vital. Ask questions – it’s your health, and you have a right to understand what’s happening. This isn’t just about interpreting a test result; it’s about safeguarding your well-being.
The Bottom Line: Empowerment and Long-Term Well-Being
A borderline ECG isn’t a death sentence. But when combined with a family history of heart problems, it serves as a valuable early warning sign. Taking charge of your heart health through open communication with your doctor, undergoing recommended tests, and making heart-healthy lifestyle changes is the best way to stay ahead of potential issues. It’s about empowerment, not fear. By being proactive, you’re making a smart investment in your long-term well-being.
How to Interpret Borderline ECG Results for Better Patient Care: A Guide
A borderline electrocardiogram (ECG) can be confusing. It’s like being on the fence – not quite normal, but not clearly abnormal either. This ambiguity makes how to interpret borderline ecg results for better patient care a critical area of focus for both patients and healthcare providers. What does it mean? What should you do next? Let’s explore.
Understanding Borderline ECG Findings
Slight variations in your heart’s electrical activity show up on an ECG. These deviations aren’t necessarily a cause for alarm. However, they require further evaluation to rule out underlying heart conditions. Think of it as a yellow traffic light – you need to proceed with caution and get more information. A 2022 study published in the European Heart Journal – Digital Health, revealed that borderline ECG findings appear in over 20% of routine ECG screenings, highlighting the importance of understanding what this means.
Family History and Borderline ECGs: Increased Risk
Your family history significantly impacts risk assessment. If heart disease runs in your family, a borderline ECG warrants even closer attention. A family history increases your risk of heart problems, making prompt investigation crucial. This doesn’t mean immediate panic; it simply emphasizes the need for further diagnostic testing.
Steps to Take with a Borderline ECG: Navigating Your Unique Situation
What’s the next step? It’s not a one-size-fits-all answer. Your doctor will consider your individual situation, including any symptoms, family history, and overall health.
- Discuss your results with your physician: This is the most crucial step. They can interpret the results in the context of your medical history.
- Undergo further testing: Your doctor might recommend additional tests like a stress test, echocardiogram, or Holter monitor (a device that records your heart’s activity over a period of time).
- Address Lifestyle Factors: Make positive lifestyle changes. Eating a heart-healthy diet, getting regular exercise, and managing stress actively reduce your risk.
- Manage underlying conditions: If you have conditions like high blood pressure or diabetes, ensure they’re well-controlled. These conditions can influence ECG results and overall heart health.
Risk Factors and Borderline ECGs: Assessing Deviation Severity
Several factors influence the interpretation of a borderline ECG.
| Factor | Low Risk | Moderate Risk | High Risk |
|---|---|---|---|
| ECG Deviation Severity | Minimal, isolated changes | Multiple minor deviations; subtle rhythm changes | Significant deviations; pronounced rhythm changes |
| Symptoms | None | Occasional mild symptoms (e.g., mild palpitations) | Frequent or severe symptoms (e.g., chest pain, shortness of breath) |
| Family History | No significant family history of heart disease | Family history of heart disease in distant relatives | Family history of early-onset heart disease in immediate family |
| Other Risk Factors | None | One or two risk factors (e.g., smoking, high cholesterol) | Multiple risk factors (e.g., diabetes, obesity, sedentary lifestyle) |
Making Informed Decisions: Empowering Yourself
Receiving a borderline ECG result can be unsettling. Focus on gathering the necessary information, discussing your results with your doctor, and actively participating in your heart health management. The good news is that advancements in AI and automation are leading to fewer cases of borderline ECG reports, with newer AI-assisted ECG machines providing more accurate results. This may result in better and more accurate treatment decisions.
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026