Low sodium in the blood (hyponatremia) can be challenging, but this comprehensive guide provides the knowledge needed to manage it effectively. We’ll explore the latest clinical guidelines, compare different treatment approaches, and provide a clear, step-by-step management plan. This resource will serve as your guide for diagnosing and treating hyponatremia. We’ll cover evidence-based practices, highlight common pitfalls, and help you remain current with the latest research, empowering you to handle hyponatremia cases with confidence and achieve optimal outcomes for your patients. For more detailed guidelines, see these treatment guidelines.
Clinical Guidelines: Mastering Low Sodium Levels & Treatment Options
Hyponatremia, characterized by low sodium levels in the blood, presents a complex clinical challenge. It’s a medical puzzle due to its diverse etiologies, ranging from simple dehydration to intricate hormonal imbalances. This guide aims to equip healthcare providers with the necessary knowledge to understand and manage hyponatremia effectively, utilizing the most current clinical guidelines. We will examine optimal diagnostic and therapeutic strategies, emphasizing established consensus and areas of ongoing investigation. A thorough understanding of the complexities of hyponatremia is essential for implementing tailored management strategies and improving patient outcomes.
Initial Assessment: Evaluating the Patient with Hyponatremia & Electrolyte Imbalance
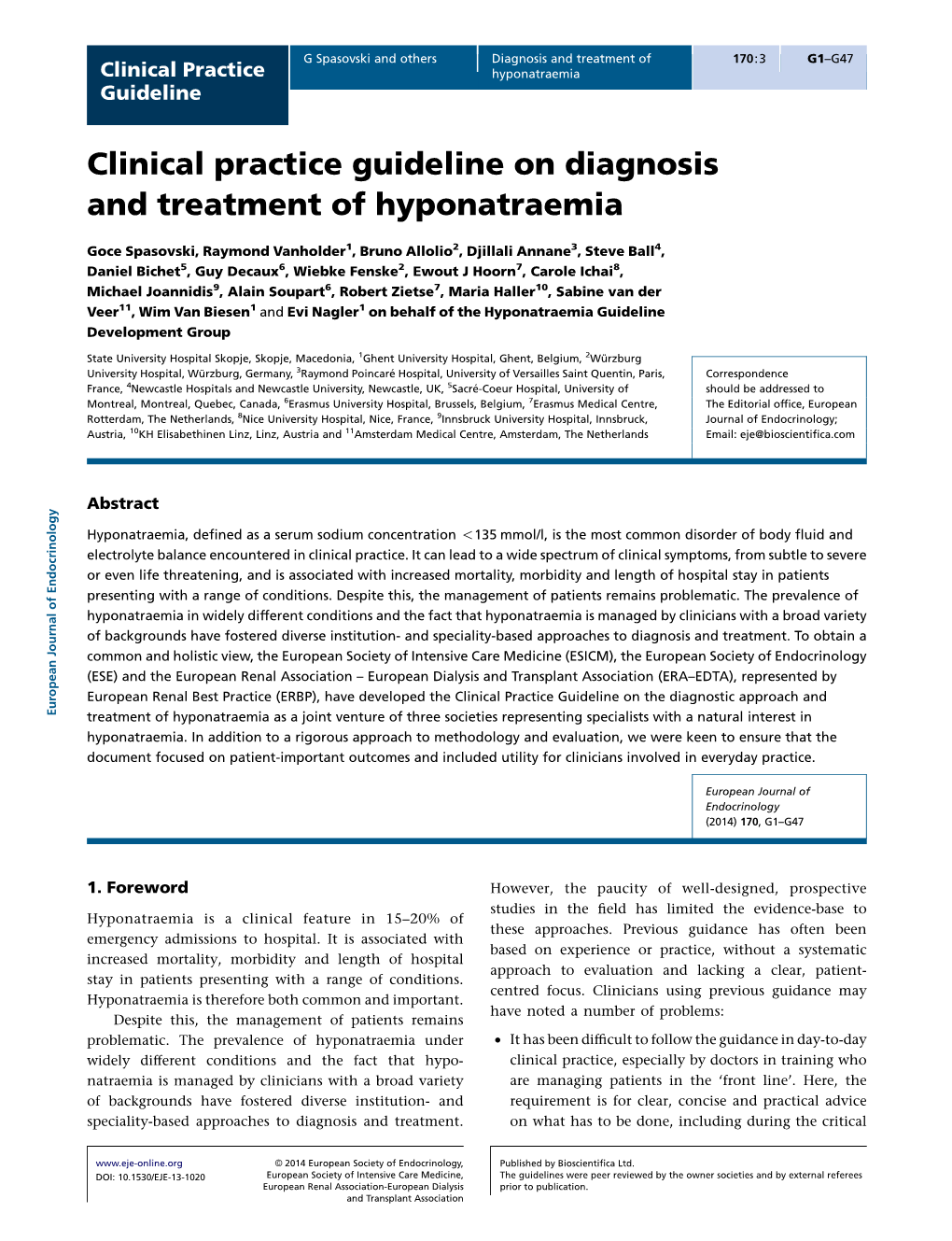
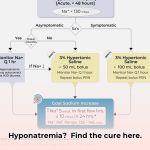
The initial patient assessment is crucial and forms the foundation of the treatment plan. Determine the patient’s fluid status—assessing for dehydration, normal fluid levels, or fluid overload. Order blood and urine tests to analyze sodium and other relevant electrolytes. This initial evaluation aids in classifying the type of hyponatremia, which is essential because treatment depends on the specific classification. An accurate initial assessment is key. Early recognition of hyponatremia, based on a patient’s medical history, physical examination, and laboratory results, allows for accurate diagnosis and timely intervention.
Diagnostic Tests: Comprehensive Sodium Level Evaluation
While consensus exists regarding the importance of measuring sodium levels in blood and urine, the necessity of other diagnostic tests remains a subject of debate. Some guidelines advocate for routine blood testing for copeptin, a surrogate marker for arginine vasopressin (AVP), a hormone that regulates water balance. Other guidelines don’t consider this test essential. This discrepancy highlights ongoing discussions within the field regarding optimal diagnostic approaches. There is no universally accepted protocol. Diagnostic accuracy is vital to differentiate between various types of hyponatremia (e.g., hypovolemic, euvolemic, hypervolemic). Further investigations may include assessing thyroid function, adrenal function, and medication review.
Treatment Strategies: A Tailored Approach & Management Plan
Treatment strategies vary depending on the underlying cause of hyponatremia. For patients with normal fluid levels, fluid restriction is often the initial intervention. However, management becomes more complex in cases of fluid overload. Treatment options may include diuretics, dietary sodium adjustments, or, in severe cases, dialysis. The optimal approach is always based on individual patient factors, their overall health, and the etiology of their low sodium levels. Evidence-based treatment should incorporate:
- Addressing the Underlying Cause: Identifying and treating the root cause of the hyponatremia, such as addressing medication side effects, hormonal imbalances, or underlying medical conditions.
- Fluid Management: Restricting fluid intake in hypervolemic hyponatremia or administering intravenous fluids cautiously in hypovolemic hyponatremia.
- Sodium Replacement: Administering sodium via oral or intravenous routes, while carefully monitoring serum sodium levels to avoid overcorrection.
- Medications: Using medications, such as vasopressin receptor antagonists (vaptans) in specific cases, to promote water excretion and increase serum sodium levels under close medical supervision.
Tailoring treatment plans based on patient-specific factors, such as age, comorbidities, and symptom severity, is essential for optimized outcomes.
Osmotic Demyelination Syndrome (ODS): Prevention Strategies & Neurological Complications
A significant concern in hyponatremia management is the risk of ODS, a potentially devastating neurological complication. All guidelines emphasize the importance of gradual sodium correction to mitigate this risk. However, the optimal rate of correction remains a topic of ongoing debate. The challenge lies in striking a balance between alleviating symptoms and preventing serious complications. Careful monitoring of sodium levels and treatment adjustments are critical for preventing ODS, ensuring patient safety, and minimizing potential neurological harm. Frequent neurological assessments are essential.
Clinical Guidelines: Concordance and Divergences & Evidence-Based Practices
A review of existing clinical guidelines reveals areas of agreement and points of divergence. Most guidelines agree on the importance of the initial assessment and the need for slow sodium correction. However, there is less consensus regarding the most valuable ancillary tests and the specific treatment protocols for certain types of hyponatremia. Therefore, clinicians must critically evaluate the guidelines and select the most appropriate approach for each patient. The need for continuous evaluation and critical application of clinical guidelines promotes personalized medicine and improved patient outcomes.
The Future of Hyponatremia Management: Ongoing Research & Clinical Research
Ongoing research efforts are aimed at refining the diagnosis and treatment of hyponatremia. Researchers are actively investigating improved diagnostic modalities and conducting large-scale clinical trials to identify the most effective treatment strategies. Developing strategies to better predict and prevent ODS is also a key focus. Progress in hyponatremia management relies on continuous clinical trials and research aimed at developing better diagnostic and therapeutic options.
Bridging the Gap: Integrating Guidelines into Practice & Patient Education
This guide provides a general overview of the key principles outlined in leading clinical guidelines for hyponatremia. Effective management involves a thorough initial assessment followed by a carefully designed, individualized treatment plan. This information is intended for educational purposes and should not replace consultation with a qualified healthcare professional. It aims to enhance healthcare providers’ understanding of the complexities of managing hyponatremia and to keep them informed about the latest clinical research and best practices. Educational initiatives for both providers and patients can improve understanding and outcomes in hyponatremia management.
Comparative Analysis of Hyponatremia Management Guidelines
| Guideline Source | Diagnostic Tests | Treatment for Hypervolemic Hyponatremia | Sodium Correction Rate |
|---|---|---|---|
| European Guidelines | Serum/urine osmolality, electrolytes, copeptin | Fluid restriction, diuretics, vaptans | ≤ 10-12 mmol/L per 24 hours, with slower rates in high-risk patients |
| US Guidelines | Serum/urine osmolality, electrolytes, hormonal assays | Fluid restriction, diuretics, sodium chloride | ≤ 8 mmol/L per 24 hours |
| UK Guidelines | Serum/urine osmolality, electrolytes | Fluid restriction, diuretics | Individualized, generally ≤ 10 mmol/L per 24 hours |
(Note: This table is a simplified comparison and does not encompass all nuances of each guideline. Clinicians should consult the full guidelines for detailed recommendations.)
Hypervolemic Hyponatremia in Cirrhosis: A Comprehensive Guide
Key Takeaways:
- Hypervolemic hyponatremia in cirrhosis results from a complex interplay of factors, including splanchnic vasodilation and inappropriate antidiuretic hormone (ADH) release.
- Fluid restriction is the initial treatment strategy.
- The use of vaptans (V2 ADH receptor antagonists) is controversial, with limited evidence supporting their widespread use due to potential risks.
- Early detection is crucial, as hyponatremia can precede more severe complications like ascites and hepatorenal syndrome (HRS).
- MELD-Na integrates sodium levels to better predict mortality and guide liver transplant prioritization.
- Careful monitoring and a tailored approach are vital to avoid rapid sodium corrections and potential neurologic complications.
Understanding Hypervolemic Hyponatremia in Cirrhosis & Liver Disease
Cirrhosis, characterized by advanced liver scarring (fibrosis), commonly leads to hypervolemic hyponatremia, a condition marked by low sodium levels despite the presence of excess fluid in the body. This phenomenon arises from a complex interaction of several factors, disrupting the body’s fluid and electrolyte equilibrium. The liver’s impaired function triggers compensatory mechanisms, resulting in fluid retention and a subsequent reduction in sodium concentration in the blood. Understanding the interrelationship between liver function and fluid balance is crucial for effectively managing hypervolemic hyponatremia.
Pathophysiology: Unraveling the Causes & Renin-Angiotensin-Aldosterone System (RAAS)
The underlying causes of hypervolemic hyponatremia are multifactorial, including:
- Splanchnic vasodilation: Dilation of blood vessels in the gut reduces effective blood volume, activating the renin-angiotensin-aldosterone system (RAAS) and the sympathetic nervous system, leading to increased sodium and water retention.
- Inappropriate ADH release: Excessive secretion of antidiuretic hormone (ADH) promotes water retention by the kidneys, further diluting the sodium concentration in the blood.
- Reduced oncotic pressure: Diminished albumin production by the failing liver reduces oncotic pressure within the blood vessels, contributing to fluid extravasation into the interstitial space.
These processes act synergistically, complicating the management of this condition. A thorough understanding of these mechanisms is essential for effective management.
Treatment Strategies: A Balanced Approach & Step-by-Step Guide
How to manage hypervolemic hyponatremia based on underlying causes requires a multi-faceted approach that prioritizes addressing the underlying issues.
- Fluid Restriction: Restricting fluid intake helps reduce the excess water volume
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026