Heart failure presents significant challenges, especially when complicated by low blood sodium levels (hyponatremia). This guide provides a breakdown of understanding, diagnosing, and treating this problem in heart failure patients, highlighting common pitfalls and providing actionable steps for improved patient care. For more on ICD-10 codes related to hyponatremia, see this helpful resource.
Congestive Heart Failure Hyponatremia: Better Outcomes Today and Tomorrow
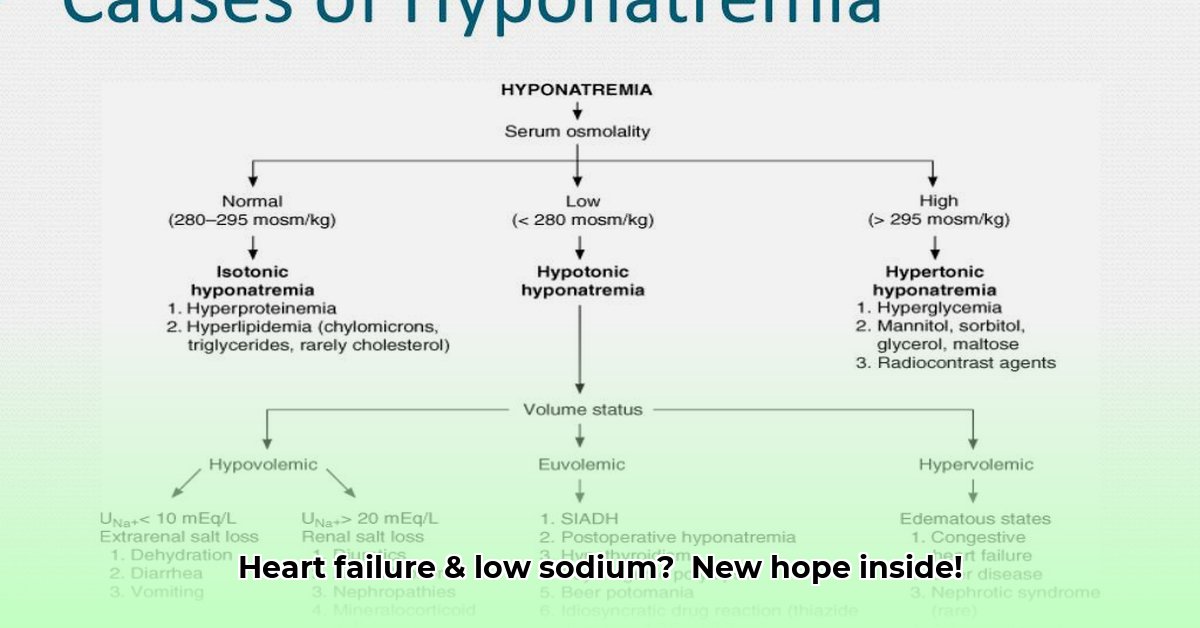
Congestive heart failure (CHF) frequently leads to hyponatremia, characterized by diminished sodium levels in the bloodstream. This intricacy arises from the body’s compensatory mechanisms, such as the persistent release of arginine vasopressin (AVP) in the setting of ineffective renal perfusion secondary to low cardiac output. Diuretics, often prescribed for CHF, can exacerbate this issue by eliminating sodium, creating a delicate balance that’s easily disrupted. It’s a multifaceted issue needing comprehensive understanding for effective resolution. The type of hyponatremia (hypervolemic vs. hypovolemic) critically influences treatment selection.
Understanding the underlying cause is critical. Is there too much fluid (hypervolemic), or too little (hypovolemic)? This directs treatment strategies, requiring tailored approaches based on fluid levels.
The Seriousness of Low Sodium in Heart Failure
Hyponatremia in CHF correlates with extended hospital stays, increased readmission rates, and elevated mortality risks, disrupting vital bodily functions. In fact, studies have shown that heart failure patients with hyponatremia were more likely to be admitted to the ICU reflecting the severity of HF and/or the direct effect of hyponatremia. It’s a complex puzzle scientists are actively solving. Does a mildly low reading always necessitate immediate intervention?
Managing and Treating Low Sodium Levels in Heart Failure
Effective hyponatremia management in CHF focuses on accurate diagnosis, understanding the root cause, and carefully adjusting diuretics.
Here’s a streamlined approach:
- Regular Monitoring: Frequent blood tests for early detection and timely intervention.
- Type Identification: Determining hypervolemic or hypovolemic status guides treatment.
- Diuretic Management: Adjusting diuretic dosage to control fluid without excessively lowering sodium.
- Fluid Balance: Modulating fluid intake based on fluid status (restriction for excess, supplementation for deficit).
- Advanced Interventions: In severe cases, medications like tolvaptan or hypertonic saline may be considered, tailored to individual needs.
The Future of Hyponatremia Management in Heart Failure
The medical community is persistently pursuing refined strategies for managing this complication through early risk identification, treatment enhancement, and innovative approaches.
Consider these objectives:
| Stakeholder | Short-Term Goals | Long-Term Goals |
|---|---|---|
| Doctors | Improve diuretic use, better identify at-risk patients. | Develop customized treatment plans, enhance understanding of mild vs. severe hyponatremia. |
| Pharmaceutical Companies | Refine current treatments, develop enhanced vasopressin blockers. | Create targeted treatments addressing the core causes of low sodium. |
| Healthcare Systems | Improve data collection, establish consistent management protocols. | Invest in research and education enhancing patient outcomes. |
Effective management requires a holistic approach across the healthcare system, continuously evolving.
How to Differentiate Hypervolemic and Hypovolemic Hyponatremia in Heart Failure Patients
Hyponatremia diagnosis, or low sodium, seriously complicates heart failure (HF) and makes the prognosis worse, so it’s important to know how to differentiate hypervolemic and hypovolemic hyponatremia in heart failure patients.
Key Takeaways:
- Hyponatremia can significantly affect the prognoses of heart failure patients.
- It occurs because of either fluid overload (hypervolemic) or fluid depletion (hypovolemic).
- Distinguishing between the two is critical for effective treatment.
- Proper diagnosis needs careful evaluation of fluid status and kidney function.
- Treatment options depend on the kind of hyponatremia.
Understanding the Problem: Hyponatremia in Heart Failure
Heart failure (HF) frequently causes hyponatremia, which is when there are low sodium levels in the blood. It has serious health consequences for patients, including increased risk of death if untreated. So, what are the two different types of hyponatremia?
Two Sides of the Same Coin: Hypervolemic vs. Hypovolemic Hyponatremia
Hyponatremia in HF usually falls into two categories: hypervolemic and hypovolemic. The difference is volume.
- Hypervolemic hyponatremia: The more common type of hyponatremia comes from fluid retention and the body holding on to too much water. In these cases, the kidneys are unable to properly excrete water, thus, diluting the sodium.
- Hypovolemic hyponatremia: Less common, stemming from inadequate blood volume due to dehydration or fluid loss, causing kidneys to reabsorb water.
The Crucial Distinction: How to Differentiate Hypervolemic and Hypovolemic Hyponatremia in Heart Failure Patients
The effective differentiation requires a clinical assessment of the patient.
-
Physical Examination:
- Look for signs of edema (swelling) or weight gain suggesting hypervolemia, versus dehydration evident through dry mucous membranes.
- Monitor blood pressure and heart rate; hypovolemia typically manifests with hypotension and tachycardia.
-
Laboratory Tests:
-
Serum sodium: Both conditions will present as low serum sodium in the blood.
- Urine sodium: Hypervolemic often means high urine sodium from the kidneys failing to excrete. Hypovolemic might mean low urine sodium.
- Urine osmolality: Assessing urine concentration. High in hypovolemic hyponatremia as kidneys retain water.
- Serum osmolality: Low serum confirms the hyponatremia diagnosis.
-
Fractional Excretion of Sodium (FENa):
-
Evaluating kidney’s ability to excrete sodium, a crucial tool for differentiation.
Treatment Strategies: Tailoring the Approach
Treatment hinges on the correct diagnosis.
- Hypervolemic hyponatremia: Managing fluid overload with diuretics (such as loop diuretics), fluid restriction.
- Hypovolemic hyponatremia: Requires fluid resuscitation with isotonic saline. Addressing the cause is essential.
Monitoring and Further Investigation
Monitor serum sodium and investigate any underlying conditions comprehensively. What co-morbidities could be contributing to both HF and hyponatremia?
Managing Hyponatremia in Acute Decompensated Heart Failure
Key Takeaways:
- Hyponatremia (low sodium) is common in ADHF and can be deadly.
- There are two types of hyponatremia: too much fluid or sodium loss.
- How to handle hyponatremia in Acute Decompensated Heart Failure (ADHF)? requires adjusting fluid intake and diuretic.
- Limiting fluids helps with hyponatremia.
- Vasopressin antagonists are being researched.
- Potassium and magnesium are essential electrolytes that need to be monitored.
Understanding the Problem: Hyponatremia and ADHF
Hyponatremia in ADHF results from disrupted fluid balance and the body’s counteraction to a failing heart, causing arginine vasopressin (AVP) to be released. Diagnosing involves determining if it’s dilutional (excess fluid) or depletional (sodium loss), crucial for treatment in Managing Hyponatremia in Acute Decompensated Heart Failure.
Diagnosing the Imbalance: More Than Just a Number
Diagnosing hyponatremia involves assessing fluid levels, kidney function, and requires a comprehensive evaluation. Does the patient have a history of heavy diuretic use? It is also important to consider underlying causes such as cardiorenal syndrome (CRS) encompasses a disorder of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction in the other organ.
Treatment Strategies: A Delicate Balancing Act
Treating means restoring sodium, which depends on volume status. Carefully managing fluid restriction is extremely important as well as diuretic therapy (prioritizing loop diuretics), while monitoring potassium levels.
The Role of Vasopressin Antagonists: A Promising but Unsettled Area
Vasopressin receptor antagonists show promise in managing fluid volume.
The Importance of Potassium and Magnesium
Monitor potassium and magnesium, replenishing if depleted.
Moving Forward: Research and Clinical Practice
Research is ongoing for better tools to manage hyponatremia. Clinicians should be aware of this.
Hyponatremia Treatment Strategies in Elderly Heart Failure Patients
Managing low sodium, or hyponatremia, can be difficult, especially for seniors. What are some options to consider in hyponatremia treatment strategies in elderly heart failure patients?
Key Takeaways:
- Hyponatremia is common in heart failure patients.
- It must be determined if it
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026