Low sodium levels caused by diuretic medications can be a concern, but understanding the issue can help manage the risks. This guide breaks down what you need to know about diuretic-induced hyponatremia, outlining the differences between types of diuretics and why some pose a higher risk. You’ll learn about preventing dangerously low sodium, avoiding common pitfalls, and managing this condition safely. This guide offers practical advice for patients and healthcare professionals alike, ensuring both understand the nuances and steps to take in various scenarios. For more information on hyponatremia ICD codes, see this useful resource.
Diuretic-Induced Hyponatremia: Understanding the Risks and Sodium Imbalance
Diuretics, or water pills, treat high blood pressure, edema, and other conditions involving excess fluid retention. However, they can sometimes lead to low sodium levels, called diuretic-induced hyponatremia. Let’s explore what this means and the associated risks, focusing on maintaining a healthy sodium balance, identifying contributing factors, and outlining management strategies.
What is Diuretic-Induced Hyponatremia?
Diuretics help the body remove excess fluid by increasing urine production. But sometimes, this process throws off the balance of water and sodium in the blood. Hyponatremia occurs when sodium levels become dangerously low (typically defined as a plasma sodium concentration below 135 mEq/L), and when caused by diuretics, it’s called diuretic-induced hyponatremia (DIH). This electrolyte imbalance can cause a spectrum of symptoms and, if left unaddressed, can lead to significant morbidity and even mortality. It’s crucial to understand both the symptoms and the underlying mechanisms to effectively manage this condition.
Thiazides and Loop Diuretics: Understanding the Differences
Not all diuretics are the same; some are more likely to cause sodium drops. Thiazide diuretics are demonstrably more prone to causing DIH than loop diuretics because they act differently in the kidneys. Loop diuretics inhibit sodium chloride reabsorption in the thick ascending limb of the loop of Henle, promoting rapid fluid removal, while thiazides work in the distal convoluted tubule, affecting smaller channels specifically involved in sodium regulation. This distinction affects how kidneys manage water and sodium, influencing the low sodium risk. The difference in action sites also impacts the body’s hormonal response, adding another layer of complexity to the risk profile.
Understanding the Body’s Response: Hormones, Kidneys, and Fluid Regulation
DIH results from a complex interaction between the body’s systems. Vasopressin, also known as antidiuretic hormone (ADH), a hormone that helps the body retain water, plays a crucial role. Diuretics, particularly thiazides, can sometimes trigger an increase in vasopressin secretion. This hormonal surge causes the body to hold onto too much water, consequently diluting the sodium in the blood. If kidneys aren’t efficiently flushing out extra water, or if there’s an underlying impairment in their diluting capacity, this worsens the problem. Drinking excessive fluids, especially hypotonic fluids, can exacerbate this dilution. Research continues to explore the intricate relationships between diuretics, hormones, and kidney function in DIH, focusing on personalized risk assessments. Furthermore, conditions like the syndrome of inappropriate antidiuretic hormone secretion (SIADH) can amplify the risk.
- Diuretics, particularly thiazides, can disrupt sodium balance, leading to hyponatremia.
- Hormonal responses, like increased vasopressin, contribute to the dilution of sodium in the blood.
- Kidney function plays a pivotal role in regulating fluid and electrolyte balance, affecting DIH risk.
Who’s Most at Risk of Developing Diuretic-Induced Hyponatremia?
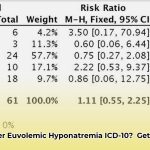
Certain individuals are more susceptible to DIH, including older adults, women, and those with a low Body Mass Index (BMI). These demographics often exhibit physiological characteristics that render them more vulnerable. Their bodies may react differently to diuretics, making them more likely to develop DIH. Additionally, individuals with pre-existing conditions or those taking multiple medications (polypharmacy) are at increased risk.
- Older adults: Their bodies often respond differently to medication due to age-related changes in kidney function and hormonal regulation.
- Women: They can have subtle differences in how their bodies handle fluid balance compared to men, possibly due to hormonal influences.
- People with a low BMI (Body Mass Index): A lower BMI might mean they have less overall fluid volume to buffer against changes, making them more sensitive to sodium fluctuations.
Is it possible that personalized medicine, tailored to individual body compositions and hormonal profiles, could mitigate the risk of DIH in these vulnerable populations? The integration of genetic markers and comprehensive metabolic panels could offer a more precise approach to diuretic therapy.
Recognizing the Warning Signs and Symptoms of Low Sodium
In many cases, DIH doesn’t cause noticeable symptoms, especially if the sodium level decreases gradually. However, severe cases with very low sodium levels (below 120 mEq/L) can cause a range of symptoms, including nausea, vomiting, headache, muscle cramps, confusion, lethargy, seizures, or even coma. If you experience these symptoms, seek immediate medical attention, especially after starting a new diuretic. Timely recognition of these symptoms can prevent severe complications. It’s also important to note that the speed at which hyponatremia develops influences the severity of symptoms.
Treatment and Prevention: A Two-Pronged Approach to Managing Sodium Levels
Treatment usually involves addressing the underlying cause, which often means reducing or stopping the diuretic and gradually increasing sodium levels under medical supervision. The approach depends on the severity and underlying cause of the hyponatremia. In mild cases, fluid restriction and monitoring may suffice. In more severe cases, intravenous saline solutions may be necessary. Limiting fluid intake may also be recommended. The best strategy is prevention; doctors closely monitor at-risk patients and consider alternative options. For patients with chronic hyponatremia, medication adjustments and dietary modifications are crucial.
Future Research: What We Still Don’t Know About Diuretic-Induced Hyponatremia
Many questions about DIH remain unanswered. Ongoing research aims to fully understand the detailed mechanisms of how DIH develops, identify who is at the highest risk, improve identification and prediction methods, and develop tailored treatments for individual patients. Specific areas of interest include the genetic predispositions to DIH and the development of novel diuretics with a lower risk profile.
Is there a potential for AI-driven predictive models to identify high-risk individuals before they even start diuretic treatment, thus preventing DIH preemptively? The integration of machine learning algorithms, leveraging patient data and pharmacological profiles, could revolutionize risk stratification.
Working Together for Better Outcomes: Stakeholder Collaboration
Addressing DIH effectively requires collaborative effort among doctors, researchers, pharmaceutical companies, patients, and regulatory agencies. A multi-faceted approach is essential to minimize its impact.
| Stakeholder | Short-Term Actions | Long-Term Actions |
|---|---|---|
| Doctors/Prescribers | Closely monitor at-risk patients; educate patients on the risk; consider alternative medications. | Invest in research to fully understand DIH; develop targeted prevention and treatment strategies; adopt personalized approaches. |
| Pharmaceutical Companies | Develop new diuretics with lower risk of DIH. | Invest in research into DIH; create better patient education materials. |
| Patients | Know your risk factors; report any unusual symptoms to your doctor immediately. | Participate in research; follow your doctor’s treatment plan carefully. |
| Regulatory Agencies | Review and update guidelines on diuretic prescribing and safety information. | Update guidelines based on new research findings; support and fund additional research studies. |
By working together, we can improve the identification, prevention, and treatment of this often-overlooked complication of diuretic use. Early detection strategies are important.
How to Prevent Thiazide-Induced Hyponatremia in Elderly Women: Prevention Strategies
Thiazide-induced hyponatremia (TIH) is a significant concern in older women taking thiazide diuretics. Several factors increase the risk, and early detection and proactive strategies are essential to avoid severe neurological complications. Prevention requires collaborative strategies from doctors and patients. A proactive approach, involving careful assessment and personalized interventions, is critical.
Understanding the Problem: The Impact of Thiazide Diuretics on Sodium
Hyponatremia, or low sodium levels, can occur as a side effect of thiazide diuretics prescribed for hypertension. This is particularly concerning in elderly women because their bodies handle fluids and electrolytes differently. Reduced kidney function and age-related changes make them more susceptible. Thiazides can disrupt the fluid balance, leading to dangerously low sodium levels, which can cause symptoms ranging from fatigue to severe neurological problems. The potential for subtle, yet debilitating, cognitive impairments makes early detection paramount.
Risk Factors: Who’s Most Vulnerable to Developing Thiazide-Induced Hyponatremia?
Several factors increase the risk of TIH in older women:
- Age and Gender: Being an older woman significantly increases the risk due to physiological changes and hormonal factors.
- Low Body Mass Index (BMI): Lower BMI correlates with increased susceptibility as it can indicate reduced fluid reserves.
- Pre-existing Conditions: Heart failure and kidney disease add significantly to the risk by impairing fluid regulation.
- Polypharmacy: The combination of thiazides with NSAIDs or SSRIs is particularly risky due to
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026