Euvolemic hyponatremia, a complex electrolyte disorder, demands precise ICD-10 coding for accurate billing and optimal reimbursement. This comprehensive guide provides a detailed, step-by-step approach to confidently navigate the coding process, minimizing errors and maximizing timely payments. We will explore the intricacies of euvolemic hyponatremia, focusing on diagnostic criteria, appropriate ICD-10 code E87.1 application, and strategies to avoid common coding pitfalls. For more information on hyponatremia coding, see this helpful resource on hyponatremia ICD-10 codes. Enhance your coding expertise, protect your revenue cycle, and ensure compliance with industry best practices.
Comprehensive Guide to Euvolemic Hyponatremia ICD-10 Coding
Mastering ICD-10 coding for euvolemic hyponatremia is not just about assigning a code; it’s about understanding the condition, its causes, and the documentation required to support accurate billing. This guide provides in-depth knowledge and actionable strategies for healthcare professionals.
Understanding Euvolemic Hyponatremia: A Delicate Balance
Euvolemic hyponatremia is characterized by low serum sodium levels (hyponatremia) despite normal extracellular fluid volume. This seemingly paradoxical condition arises when excess water dilutes the sodium concentration in the blood. The causes of euvolemic hyponatremia are diverse, ranging from hormonal imbalances to medication side effects. Recognizing the underlying etiology is key to accurate diagnosis and coding.
Symptoms of euvolemic hyponatremia can vary widely, from subtle neurological changes like mild headaches and fatigue to more severe manifestations such as confusion, seizures, and even coma. Early and accurate diagnosis is critical to prevent complications.
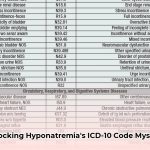
ICD-10 Code E87.1: Low Sodium in Context
The primary ICD-10 code for euvolemic hyponatremia is E87.1, representing hypo-osmolality and hyponatremia. While this code indicates low sodium levels, its application requires careful consideration of the patient’s fluid status and a thorough evaluation to rule out other potential causes of hyponatremia. Using E87.1 correctly involves more than just identifying a low sodium level; it demands a holistic assessment of the patient’s condition.
Diagnosing Euvolemic Hyponatremia: Unraveling the Mystery
Diagnosing euvolemic hyponatremia requires a systematic approach, much like a detective piecing together clues. Here’s a step-by-step guide:
- Assess Clinical Presentation: Begin by carefully evaluating the patient’s symptoms. Common symptoms include nausea, headache, lethargy, muscle cramps, and altered mental status. The severity of symptoms often correlates with the rate and degree of sodium decline.
- Confirm with Laboratory Findings: Blood tests are essential to confirm the diagnosis. A serum sodium level below 135 mEq/L is indicative of hyponatremia. Serum osmolality should also be measured to confirm hypo-osmolality (typically below 280 mOsm/kg).
- Evaluate Fluid Status: Assess the patient’s fluid status to differentiate euvolemic hyponatremia from hypovolemic (dehydration) or hypervolemic (fluid overload) hyponatremia. Look for signs of edema, jugular venous distention, and assess skin turgor.
- Identify the Underlying Cause: Determining the underlying cause of euvolemic hyponatremia is critical. Common causes include Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH), hypothyroidism, adrenal insufficiency, and certain medications (e.g., diuretics, selective serotonin reuptake inhibitors).
- Rule Out Other Conditions (Differential Diagnosis): Exclude other conditions that can mimic euvolemic hyponatremia, such as pseudohyponatremia (falsely low sodium due to elevated lipids or proteins) and hyperglycemia-induced hyponatremia.
Documentation Essentials for Accurate Coding
Comprehensive and accurate documentation is the cornerstone of compliant coding. Key elements to include in the patient’s medical record include:
- Detailed Description of Symptoms: Be specific about the patient’s symptoms, including their onset, duration, and severity.
- Relevant Laboratory Data: Include serum sodium levels, serum osmolality, urine osmolality, and any other relevant lab results.
- Assessment of Fluid Status: Clearly document the patient’s fluid status, noting the absence of edema or dehydration.
- Explanation of Differential Diagnosis: Detail the rationale for ruling out other potential causes of hyponatremia.
- Identification of Underlying Cause: Clearly state the underlying cause of euvolemic hyponatremia, if identified.
- Treatment Plan: Document the treatment plan, including fluid restriction, medication adjustments, and monitoring parameters.
Avoiding Common Coding Errors
Several common coding errors can lead to claim denials and audits. Be aware of these pitfalls:
- Confusing Hyponatremia Types: Ensure you correctly differentiate euvolemic hyponatremia from other types of hyponatremia (hypovolemic, hypervolemic). Each type has its own specific ICD-10 code.
- Inadequate Documentation: Insufficient documentation is the primary cause of coding errors. Provide enough details to support the diagnosis and coding choices.
- Failing to Identify the Underlying Cause: Neglecting to identify and code the underlying cause of hyponatremia results in incomplete coding and can impact reimbursement.
- Using Incorrect Sequencing: Code the underlying cause of hyponatremia first, followed by the code for hyponatremia (E87.1).
The Financial Implications of Accurate Coding
Accurate ICD-10 coding directly impacts reimbursement efficiency, reduces claim denials, and minimizes the risk of audits. Correct codes facilitate timely payments and ensure appropriate compensation for services rendered. Thorough documentation protects against audits and supports the medical necessity of treatment.
Real-World Case Study: Accurate Coding in Action
A 65-year-old patient presents with persistent fatigue, mild confusion, and muscle cramps. Physical examination reveals no signs of edema or dehydration. Laboratory tests reveal a serum sodium level of 128 mEq/L and low serum osmolality. Further evaluation reveals the patient is taking a selective serotonin reuptake inhibitor (SSRI) for depression. The physician determines that the SSRI is the likely cause of the euvolemic hyponatremia.
The correct ICD-10 coding for this case would be:
- T43.205A: Adverse effect of selective serotonin reuptake inhibitors, initial encounter
- E87.1: Hypo-osmolality and hyponatremia
This case highlights the importance of identifying the underlying cause of hyponatremia (in this case, the SSRI medication) and coding it appropriately.
This guide provides a general overview of ICD-10 coding for euvolemic hyponatremia. Always consult the latest ICD-10 guidelines and coding manuals for the most up-to-date information. This information is for educational purposes only and should not be considered medical or coding advice.
Preventing E87.1 ICD-10 Coding Audits for Hyponatremia: A Proactive Approach
Key Takeaways:
- Comprehensive Documentation: Detailed documentation is your first line of defense against audits. Treat the medical chart as a legal document that supports your coding choices.
- Understanding Euvolemic Hyponatremia: Grasp the nuances of euvolemic hyponatremia to ensure accurate coding. Focus on understanding why the sodium levels are low and the underlying physiological mechanisms.
- Correct Sequencing: Proper sequencing of codes is crucial for compliance. Always code the underlying cause of hyponatremia first, followed by E87.1.
- Clear Communication: Foster clear and direct communication between clinicians and coders. Ensure that coders have access to all relevant clinical information.
- Continuous Education: Stay informed about updated ICD-10 guidelines and coding best practices. Continuously educate your staff on proper coding procedures.
Deciphering ICD-10 Code E87.1: The Devil is in the Details
ICD-10 code E87.1 for hyponatremia requires precise documentation for accurate application. Simply noting “hyponatremia” is insufficient. You must specify the type of hyponatremia (euvolemic, hypovolemic, hypervolemic), its severity, and all related symptoms.
Key Diagnostic Criteria: Essential Elements for Coding
Diagnosing euvolemic hyponatremia involves a multi-faceted approach. It includes clinical observation of symptoms like nausea, lethargy, and confusion, alongside lab results confirming low serum sodium. Further investigations may include assessing urine osmolality and checking hormone levels to pinpoint the underlying cause.
Proper Documentation: Your Shield Against Audits
Accurate medical coding relies on meticulous documentation. Clear and comprehensive documentation can prevent claim denials and potential overpayments. The coder needs a complete picture of the patient’s condition. Here’s a structured approach:
- Clearly State the Diagnosis: “Euvolemic hyponatremia secondary to [cause, e.g., SIADH].”
- Document Serum Sodium Levels: Include precise numerical values and the date and time the test was performed.
- Describe the Clinical Presentation: Note all observed symptoms, including their severity and duration.
- Specify Treatments: Document all treatments administered, including fluid restriction, medication adjustments, and supportive care.
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026