Life with a tracheostomy presents unique challenges, but Heat and Moisture Exchangers (HMEs) can significantly enhance your comfort and overall quality of life. This comprehensive guide explains how HMEs function, explores the various types available, and offers clear, easy-to-follow instructions for their proper use and maintenance. It is designed for patients, caregivers, and healthcare professionals alike. Let’s begin breathing easier, together!
HME Trach: Maximizing Comfort and Lung Health
Comfortable breathing is essential for a fulfilling life, particularly when living with a tracheostomy. HMEs serve as a personal climate control system for your lungs, facilitating breathing that is both easier and more comfortable. What specific benefits do HME trach systems offer patients?
Understanding HME Trachs: Replicating Natural Humidification
The natural process of breathing involves your nose and mouth warming and humidifying the air you inhale. A tracheostomy bypasses this essential system, resulting in the inhalation of dry, often irritating air. An HME trach acts as a compact substitute for your natural system, mitigating dryness, reducing coughing, and guarding against potential lung infections by delivering added warmth and essential moisture. According to leading respiratory therapists, warm, moist air provides a superior breathing experience compared to the discomfort of cold, dry air.
Selecting the Right HME Trach System: Key Factors
Choosing the ideal HME is critical to ensure optimal comfort and effectiveness. Your healthcare provider will evaluate several factors, including the type of your tracheostomy tube (cuffed or cuffless), the HME’s filter capacity, and its breathing resistance. The most effective HME system is the one that is tailored to your specific needs and provides maximum comfort.
Effective Use of Your HME Trach: Maintenance and Prevention Strategies
Proper HME usage combined with regular maintenance is paramount. Consistently monitor for any mucus buildup and promptly replace any clogged HMEs to prevent breathing difficulties. Your healthcare team will establish specific cleaning and replacement schedules, which are essential for preventing complications and ensuring the smooth, effective operation of your device. Regular replacement is not just recommended; it’s a key preventative measure against potential complications, ensuring consistent and reliable performance.
Navigating Potential Challenges: Troubleshooting Common Issues
While HMEs offer substantial benefits, it’s important to acknowledge and address potential issues. Blocked filters can elevate breathing resistance, and certain medications may induce airway constriction. Should you experience increased breathing difficulty, excessive mucus production, or any unusual symptoms, seek immediate consultation with your healthcare provider. Close monitoring is particularly important when using mucolytic medications to reduce the risk of blockage.
Monitoring and Maintenance: Proactive Respiratory Care
Consistent monitoring and proactive care through scheduled replacements are crucial to prevent significant respiratory issues. Remember, proactive observation is often the most effective form of care. What is the easiest way to determine when your HME requires replacement?
HME Trachs and Holistic Well-being: Enhancing Quality of Life
Comfortable breathing profoundly influences your overall quality of life, and HMEs are instrumental in achieving this. To maximize their benefits, it’s essential to adhere to proper usage guidelines, maintain the device diligently, and maintain open communication with your healthcare team. Never underestimate the value of an ongoing dialogue with your healthcare providers.
Pros and Cons at a Glance: Making Informed Decisions
| Pros | Cons |
|---|---|
| Enhanced comfort and easier breathing | Potential for blockage and increased airflow resistance |
| Reduced infection risk | Requires regular monitoring and replacement |
| Cost-effective humidification | May not be suitable for all individuals |
| Simple and intuitive to use | Effectiveness can vary from person to person |
Collaborative Care: Partnering with Experts for Optimal Results
Your healthcare team is an invaluable resource throughout your HME journey. Regular checkups are essential and any concerns or changes should be promptly addressed. They form a crucial part of your support network, ensuring your HME use is both effective and comfortable. Partner with your medical team so they can fully support your care and well-being.
Choosing the Best HME for Tracheostomy Patients
Key Takeaways:
- HMEs are crucial for tracheostomy patients, replicating the natural warming and humidifying functions of the upper airway.
- The correct HME is selected based on individual patient needs, breathing support requirements, tracheostomy tube type, and desired features.
- Continuous monitoring and immediate intervention for any breathing difficulties are critical for achieving optimal patient outcomes.
- Effective HME use and management are enhanced through collaboration between patients, caregivers, and healthcare providers.
Understanding Heat and Moisture Exchangers (HMEs) Deeply
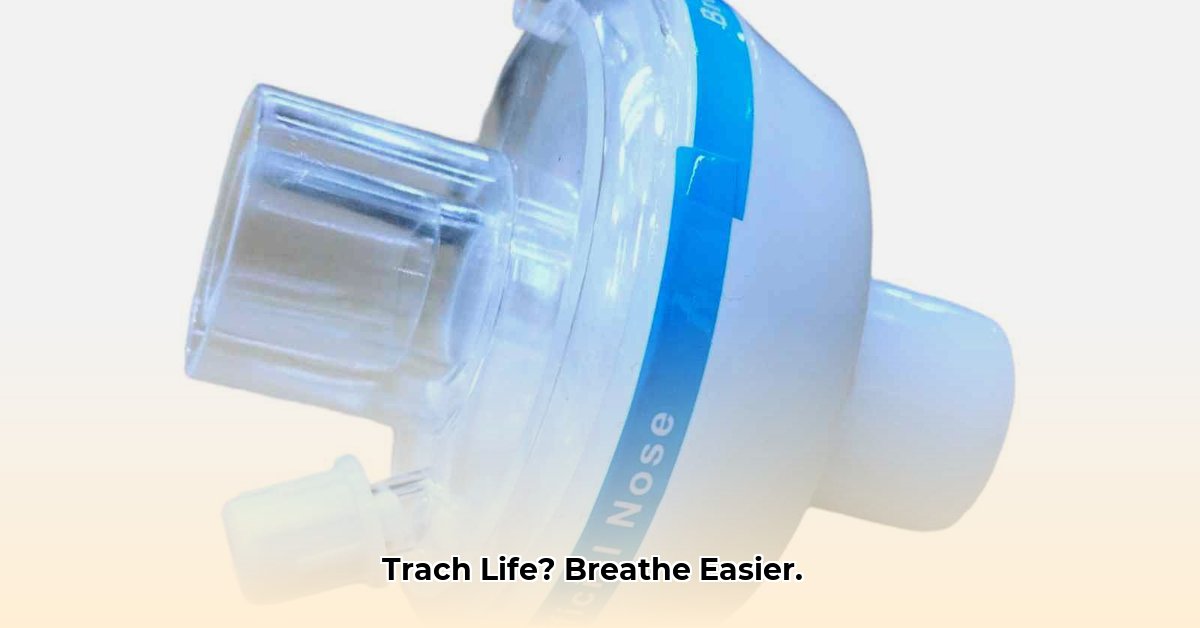
HMEs are compact, often disposable devices engineered to warm and humidify air for tracheostomy patients. They are indispensable because tracheostomies bypass the body’s natural humidification processes provided by the nose and mouth. This leads to dry air irritating the lungs, increasing mucus production, and potentially elevating the risk of infection. HMEs mitigate these issues by functioning like miniature air conditioners for the lungs, offering a more comfortable and significantly healthier breathing experience. How familiar are you with the diverse range of HME brands available in today’s market?
A Step-by-Step Guide: Selecting the Best HME for Tracheostomy Patients
Selecting the most suitable HME should be a thoughtful and customized process, not a generic, one-size-fits-all solution. To effectively navigate this decision:
- Consult Your Healthcare Team: This is the most critical step, involving a comprehensive assessment by your doctor or respiratory therapist to determine your unique requirements and recommend the most appropriate HME.
- Consider HME Types: Based on your clinician’s guidance, choose from various types, including foam, paper, or HMEFs (equipped with filters).
- Assess Breathing Comfort: Closely monitor your breathing post HME use, noting any variations and reporting them promptly to your healthcare provider.
- Proper Placement and Maintenance: Fully adhere to your healthcare team’s instructions concerning insertion and ongoing maintenance.
- Ongoing Monitoring: Maintain continuous monitoring to ensure comfortable breathing and keep open lines of communication with your healthcare team.
Important HME Features to Consider
| Feature | Description | Considerations |
|---|---|---|
| HME Type | Includes foam or paper options, as well as HMEFs enhanced with filters | Foam HMEs are generally more economical, while HMEFs provide superior protection against infections. |
| Speaking Valve Compatibility | Certain HMEs are specifically designed to function with speaking valves | This functionality is exclusively available with a cuffless tracheostomy tube. |
| Oxygen Delivery | Selected HMEs are capable of supporting supplemental oxygen | This is crucial if you require additional oxygen to support your breathing. |
| Resistance | HMEs can increase airway resistance to varying degrees, depending on the particular design | Healthcare providers need to carefully evaluate this aspect, especially for patients with pre-existing compromised breathing capabilities. |
Potential Complications and Solutions Detailed
Identifiable complications include amplified airway resistance (leading to increased breathing difficulty) and heightened mucus accumulation. Early detection and proactive communication are essential. Solutions might include modifications to the HME type, adjustments to the replacement schedule, or exploring other management strategies.
Choosing the optimal HME for tracheostomy patients is a collaborative endeavor. Engage actively with your healthcare team to improve your breathing comfort and overall respiratory health.
Comprehensive Guide: HME Trach Use in Pediatric Tracheostomy Patients
Key Takeaways:
- Maintaining adequate humidification is essential in preventing thick secretions and minimizing respiratory complications in children with tracheostomies. Various methods are available, including the use of HMEs.
- Suctioning should be performed only when clinically necessary, using meticulous technique to minimize any potential trauma.
- The frequency of tracheostomy tube changes and specific cleaning protocols can vary considerably, emphasizing the need for definitive guidelines and continued research.
- Differences exist in the proper cleaning methods for both reusable tracheostomy tubes and inner cannulas. Compliance with manufacturers’ instructions is essential.
- Infants and toddlers present unique handling challenges due to their smaller airways.
- The provision of comprehensive caregiver training and support is crucial for effective home tracheostomy management.
Understanding Heat and Moisture Exchangers (HMEs) Profoundly
HMEs function as artificial noses, effectively warming and humidifying the air your child breathes. This action prevents the drying of the airway, a particularly vital consideration for children due to their smaller airways. Envision an HME as a highly efficient and compact humidifier, conveniently positioned directly on the tracheostomy tube.
What advantages do HMEs provide compared to other humidification methods, especially within the context of pediatric care?
Advantages of HMEs in Pediatric Tracheostomy Care:
- Enhanced Comfort: Delivering humidified air is gentler on the sensitive airways of children.
- Reduced Secretions: Humidified air helps thin and loosen thick secretions, easing clearance.
- Ease of Use: HMEs are designed for easy and straightforward attachment and operation.
- Portability: HMEs greatly simplify a child’s mobility.
Considerations When Using HMEs in Pediatric Tracheostomy Care:
- Blockage Risk: Regular monitoring and replacement are required to prevent potential clogging of the device.
- Not Universally Suitable: HMEs are not appropriate for all patients, particularly those with
- The TM Book Offers an Essential Guide to Meditation. - March 4, 2026
- Transcendental Meditation Books Guiding Your Journey to Deeper Practice - March 3, 2026
- Your TM Meditation Book Explores Its Benefits and History - March 2, 2026