Accurate medical billing is essential for healthcare providers, and miscoding electrolyte disorders can lead to claim denials and audits. This comprehensive guide provides a detailed approach to mastering ICD-10 codes for electrolyte imbalances, specifically focusing on the E87 code range. Whether you’re an experienced medical coder or new to the field, this guide will equip you with the knowledge and skills needed to code confidently and ensure appropriate reimbursement for services rendered. For more on hyponatremia, see this helpful guide: Hyponatremia ICD-10.
Coding Electrolyte Disorders: Mastering the ICD-10-CM E87 Codes
This guide explores electrolyte disorders and provides detailed instructions on how to code them accurately using the ICD-10-CM system. Correct coding is not only crucial for appropriate patient care but also for ensuring proper reimbursement from insurance providers. The primary focus will be on the E87 codes, which form the cornerstone of coding for these imbalances.
The Body’s Balancing Act: Understanding Electrolyte Imbalances
Consider the human body as a complex, finely tuned machine. Electrolytes, including sodium, potassium, calcium, magnesium, chloride, phosphate, and bicarbonate, are essential for its smooth and efficient operation. These electrolytes play a critical role in maintaining fluid balance, nerve and muscle function, acid-base balance, and numerous other physiological processes. Imbalances in these electrolytes can range from mild discomfort to severe, life-threatening health issues. Therefore, accurate coding is paramount to ensuring correct patient care and appropriate reimbursement for medical services.
Common electrolyte imbalances include:
- Hypernatremia (High Sodium): Often caused by dehydration due to insufficient water intake, excessive sweating, diarrhea, or certain medications. It can also be a consequence of diabetes insipidus, which impairs the body’s ability to conserve water.
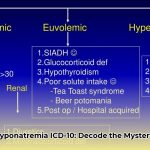
- Hyponatremia (Low Sodium): Can occur when excessive water dilutes sodium levels, potentially due to excessive water intake, kidney or heart failure, SIADH (syndrome of inappropriate antidiuretic hormone secretion), or certain medications like diuretics.
- Hyperkalemia (High Potassium): Frequently linked to kidney problems, which regulate potassium levels, and can interfere with heart rhythm, potentially leading to cardiac arrhythmias. Other causes include certain medications (e.g., ACE inhibitors, ARBs), Addison’s disease, and rhabdomyolysis.
- Hypokalemia (Low Potassium): Can lead to muscle weakness, fatigue, and heart problems, as potassium is essential for muscle function and maintaining a regular heart rhythm. Common causes include diuretic use, vomiting, diarrhea, and certain kidney disorders.
- Hypercalcemia (High Calcium): Often related to hyperparathyroidism (overactive parathyroid glands) or certain cancers that release substances increasing calcium levels in the blood. It can potentially lead to kidney stones, bone pain, muscle weakness, and confusion.
- Hypocalcemia (Low Calcium): Essential for bone health, muscle function, and blood clotting, low calcium may cause muscle cramps, numbness, tingling, and in severe cases, seizures or cardiac arrhythmias. Common causes include vitamin D deficiency, hypoparathyroidism, kidney disease, and certain medications.
- Acidosis (Too Much Acid): Occurs when the body’s pH becomes too acidic (below 7.35), potentially stemming from conditions like diabetes (diabetic ketoacidosis), kidney failure, severe respiratory issues, or lactic acidosis due to intense exercise or shock.
- Alkalosis (Too Much Base): The opposite of acidosis, where the body becomes too alkaline (above 7.45), possibly due to severe vomiting, hyperventilation, certain medications (e.g., excessive antacid use), or hormonal disorders.
Understanding the diverse causes and potential implications of each electrolyte imbalance is a foundational step toward mastering accurate coding using the ICD-10-CM system.
ICD-10-CM E87 Codes: Your Detailed Coding Roadmap
The ICD-10-CM E87 codes are essential for accurately coding electrolyte disorders. This section provides a detailed breakdown of key codes and offers guidance on selecting the most appropriate code for each specific clinical scenario.
The following table provides a comprehensive overview of common disorders of fluid, electrolyte, and acid-base balance:
| Code | Description | Common Causes/Examples |
|---|---|---|
| E87.0 | Hyperosmolality and hypernatremia | Severe dehydration (e.g., due to inadequate fluid intake, excessive sweating, diarrhea), diabetes insipidus, excessive sodium intake (e.g., from intravenous fluids), certain medications (e.g., diuretics). |
| E87.1 | Hyponatremia | Diuretic use, kidney disease, excessive water intake (e.g., psychogenic polydipsia), heart failure, liver cirrhosis, SIADH (syndrome of inappropriate antidiuretic hormone secretion), certain medications. |
| E87.20 | Acidosis, unspecified | Used when the specific type of acidosis is not documented. |
| E87.21 | Acute metabolic acidosis | Diabetic ketoacidosis (DKA), lactic acidosis, severe diarrhea, kidney failure, poisoning (e.g., salicylate overdose). |
| E87.22 | Chronic metabolic acidosis | Chronic kidney disease, renal tubular acidosis, prolonged diarrhea. |
| E87.29 | Other acidosis | Respiratory acidosis, high anion gap metabolic acidosis |
| E87.3 | Alkalosis | Severe vomiting, hyperventilation (e.g., due to anxiety or panic attacks), excessive antacid use, certain hormonal disorders (e.g., hyperaldosteronism). |
| E87.4 | Mixed disorder of acid-base balance | Complex clinical scenarios involving both acidosis and alkalosis, often seen in critically ill patients with multiple organ system dysfunction. |
| E87.5 | Hyperkalemia | Kidney failure, certain medications (e.g., ACE inhibitors, ARBs, potassium-sparing diuretics), Addison’s disease, rhabdomyolysis, metabolic acidosis. |
| E87.6 | Hypokalemia | Diuretic use, inadequate potassium intake, vomiting, diarrhea, certain kidney disorders (e.g., renal tubular acidosis), hyperaldosteronism, magnesium deficiency. |
| E87.70 | Fluid overload, unspecified | Use when the specific cause of fluid overload is not identified. |
| E87.71 | Transfusion associated circulatory overload (TACO) | Fluid overload as a direct result of blood transfusion . |
| E87.79 | Other fluid overload | Heart failure, kidney disease, liver cirrhosis, excessive intravenous fluid administration. |
| E87.8 | Other disorders of electrolyte and fluid balance, NEC | Includes conditions not classified elsewhere, such as hyperchloremia (elevated chloride levels) and hypochloremia (low chloride levels), as well as imbalances of magnesium, phosphate, and other electrolytes. |
| E87.9 | Unspecified disorder of electrolytes | Use only when absolutely no other information is available to specify the type of electrolyte imbalance. This code should be avoided whenever possible. |
It is essential to meticulously review the “Excludes1” and “Excludes2” notes in the official ICD-10-CM manual. These notes provide crucial guidance and help prevent coding errors by clarifying which conditions should not be coded together or when an alternative, more specific code should be used. For example, diabetes insipidus is excluded from E87.0 (hypernatremia) because it has a specific ICD-10-CM code (E23.2) that should be used instead.
Avoiding Common Coding Pitfalls for Accurate and Compliant Billing
Accurately coding electrolyte disorders requires meticulous attention to detail. Here are common mistakes to avoid to ensure you have the most comprehensive and accurate codes for fluid, electrolyte, and acid-base imbalances.
- Ignoring the Underlying Cause: It is crucial to code both the electrolyte imbalance and the underlying medical condition contributing to the imbalance. For example, if a patient has hypokalemia (E87.6) due to diuretic use, both the hypokalemia and the diuretic use should be coded to provide a complete clinical picture.
- Missing the Severity: The documentation should clearly reflect whether the electrolyte imbalance is acute (sudden onset) or chronic (long-lasting), as this distinction can impact coding and treatment decisions.
- Focusing Only on Symptoms: Coding should be primarily based on objective laboratory results (e.g., serum electrolyte levels) rather than solely relying on the patient’s reported symptoms. While symptoms are important for clinical assessment, lab values provide definitive evidence of an electrolyte imbalance.
- Failing to Consider Specificity: Always strive to use the most specific ICD-10-CM code available to accurately represent the patient’s condition. For example, if the medical record specifies “acute metabolic acidosis,” use E87.21 rather than the more general code E87.20 (“Acidosis,
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026