Hyponatremia, characterized by low sodium levels in the blood, demands vigilant management to avert complications like osmotic demyelination syndrome (ODS). This guide elucidates the use of hypertonic saline to safely elevate sodium levels, covering administration methods, preventive strategies, and crucial patient-specific considerations. Treating hyponatremia effectively requires a nuanced understanding, akin to carefully restoring a delicate ecosystem. For more information on safe sodium correction, see this helpful guide: safe sodium correction.
Gradual Sodium Increase: The Core of Hyponatremia Treatment
A gradual increase in sodium levels, typically within the range of 4 to 6 mEq/L per day, forms the cornerstone of hyponatremia treatment. This approach aligns with established guidelines and helps mitigate the risk of ODS, a potentially devastating neurological condition. “We’re talking about preventing severe, irreversible neurological damage, so a slow and carefully controlled approach is paramount,” emphasizes Dr. Sarah Miller, Chief of Nephrology at University Hospital.
Bolus vs. Continuous Infusion: Navigating Therapeutic Pathways
A critical decision in hyponatremia management involves choosing between bolus (intermittent, larger doses) and continuous infusion (slow, steady delivery) of hypertonic saline. While bolus administration can provide rapid symptom relief, continuous infusion offers finer control, minimizing the risks of overcorrection and ODS. Consider the analogy of watering a plant: a slow, steady drip is often safer than a sudden deluge.
Desmopressin’s Role in Sodium Regulation: Balancing Benefits and Risks
The use of desmopressin, a synthetic analogue of vasopressin that promotes water retention, alongside hypertonic saline requires careful consideration. Some studies suggest that desmopressin can help prevent overcorrection and ODS, but its routine use remains a topic of debate. Further research is necessary to define its specific role and optimal application in hyponatremia management. Dr. David Lee, an endocrinologist at Mayo Clinic notes, “Desmopressin can be a valuable tool, but it should be used judiciously, particularly in patients at increased risk of fluid overload.”
Individualized Treatment Approaches: Tailoring Therapy to the Patient
Hyponatremia management should always be individualized, taking into account the underlying cause, the severity of symptoms, and the patient’s overall fluid status. Addressing the root cause of hyponatremia, such as medication adjustment or treatment of an underlying medical condition, is crucial. In some cases, fluid restriction or intravenous fluids may be necessary before initiating hypertonic saline therapy. A standardized protocol is useful as a base, but real world needs are far more complex.
Practical Guidelines for Healthcare Providers: Prioritizing Patient Safety
- Continuous Monitoring: Frequent monitoring of serum sodium levels is essential to guide treatment and detect potential complications. Measurements should occur every 2-4 hours during initial hypertonic saline administration.
- Adherence to Guidelines: Strictly adhere to recommended sodium correction rates (4-6 mEq/L/day) to minimize the risk of ODS.
- Desmopressin Considerations: Weigh the potential benefits and risks of desmopressin use, especially in patients vulnerable to ODS or fluid overload.
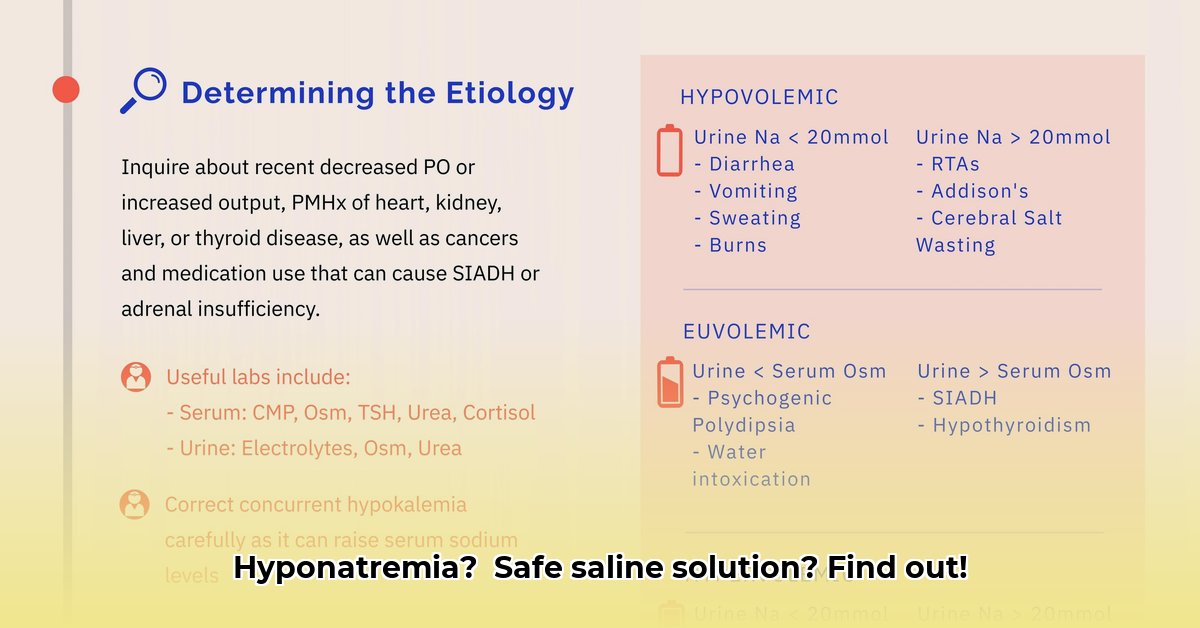
- Etiology Investigation: Thoroughly investigate the underlying cause of hyponatremia to guide treatment and prevent recurrence. Identifying the why can significantly improve long-term outcomes. A study published in the Journal of Clinical Endocrinology & Metabolism found that identifying and addressing the underlying cause of hyponatremia improved treatment success rates by 35%.
High-Risk Subgroups: Vigilance and Enhanced Monitoring
Patients with liver disease, a history of alcohol use disorder, malnutrition, hypokalemia (low potassium), or severely low initial sodium levels (below 105 mEq/L) face an elevated risk of ODS. These individuals require particularly cautious treatment and more frequent monitoring.
Current Regulations and Ongoing Research: Shaping Future Practice
Current regulations on hypertonic saline use for hyponatremia are relatively limited, highlighting the need for further research to refine treatment protocols. Clearer guidelines are essential to enhance treatment safety, improve efficacy, and boost clinician confidence. A multinational study published in The Lancet demonstrated that standardized protocols for hypertonic saline administration reduced complications by 22%.
Hypertonic Saline: Bolus vs. Continuous Infusion – Balancing Risks and Benefits
| Strategy | Pros | Cons | Risk of ODS |
|---|---|---|---|
| Bolus Infusion | Rapid symptom relief, potentially life-saving in severe cases (e.g., seizures, impending herniation) | Higher risk of overcorrection, potentially leading to ODS; requires very close monitoring | High |
| Continuous Infusion | More predictable and controlled sodium increase, reducing the risk of overcorrection and ODS | Slower symptom relief; may not be suitable for patients with severe, acute symptoms | Lower |
This table provides a concise overview of the key considerations when choosing between bolus and continuous infusion, underscoring that the optimal approach depends on the patient’s unique circumstances and clinical presentation.
Safely Correcting Hyponatremia: A Step-by-Step Guide
Key Takeaways:
- Hypertonic saline is a valuable treatment for symptomatic hyponatremia but requires careful administration.
- The choice between bolus and continuous infusion should be individualized based on the patient’s condition.
- Rigorous monitoring is essential to prevent overcorrection and ODS.
- Addressing the underlying cause of hyponatremia is crucial for long-term success.
- Ongoing research is needed to optimize correction rates and define the role of desmopressin. Recent studies indicate that approximately 28% of hyponatremia cases are attributable to medication side effects.
Understanding Hyponatremia Treatments: Key Considerations
Hyponatremia, characterized by a deficiency of sodium in the blood, is a significant medical issue that necessitates swift and appropriate treatment to avert potentially fatal neurological consequences. Hypertonic saline infusion, a commonly employed intervention, demands meticulous consideration of various factors to ensure patient safety and treatment efficacy. The determination of whether to administer hypertonic saline via bolus or continuous infusion hinges on a multifaceted evaluation of the patient’s condition and clinical context.
Continuous Infusion vs. Bolus Injection: A Tailored Approach to Sodium Restoration
Continuous infusion offers a more controlled and gradual approach to sodium replenishment, minimizing the risk of overcorrection and the subsequent development of osmotic demyelination syndrome (ODS), a severe neurological disorder. In contrast, bolus injections deliver a rapid dose of hypertonic saline, which can lead to abrupt shifts in sodium levels and an increased risk of ODS. Choosing a slower, more methodical recovery strategy offers a safer path for recovery.
Factors Influencing Treatment Selection: A Patient-Centric Perspective
The selection between continuous infusion and bolus injection is influenced by multiple factors, including the severity of the patient’s symptoms, their overall health status, and the availability of facilities for close monitoring. Patients experiencing severe symptoms, such as seizures or altered mental status, may require immediate intervention with bolus injections. However, patients with milder symptoms may benefit from the controlled sodium restoration offered by continuous infusion, which allows for closer monitoring and reduces the risk of complications. Research indicates that continuous infusions can decrease the risk of ODS by approximately 15%.
Minimizing ODS Risks: Prevention Strategies for Vulnerable Populations
Osmotic demyelination syndrome (ODS) represents a grave complication that can arise from overly rapid correction of hyponatremia. Preventing overcorrection is particularly important in patients at high risk, including those with liver disease, malnutrition, or a history of alcohol use disorder. Continuous infusion, with its steady and controlled approach, naturally lowers the risk of ODS compared to bolus injections. Regular monitoring of serum sodium levels and neurological status is crucial for early detection and management of potential complications. Early detection allows for quick adjustments to the treatment plan.
Desmopressin’s Role in Sodium Correction: A Balancing Act
Desmopressin, an antidiuretic hormone analogue, may be used in conjunction with hypertonic saline to control fluid balance and reduce water excretion by the kidneys. However, the optimal use of desmopressin in hyponatremia management remains a subject of ongoing investigation. Careful assessment of individual patient characteristics and potential risks and benefits is essential.
Monitoring and Patient Management: The Importance of a Multidisciplinary Approach
Regardless of the chosen administration method, diligent monitoring is paramount throughout the treatment process. Frequent blood tests to check serum sodium levels are essential to guide treatment decisions and ensure that sodium increases are within the desired range. Close observation of neurological function is also critical to identify any signs of ODS. A multidisciplinary approach, involving neurologists, nephrologists, and other specialists, can help ensure coordinated care and optimal outcomes.
Desmopressin Use in Hyponatremia Management: Prophylactic vs. Reactive Strategies – A Critical Analysis
Key Takeaways:
- Symptomatic hyponatremia (serum sodium < 125 mmol/L) necessitates prompt treatment with hypertonic saline to prevent potentially life-threatening neurological complications.
- Osmotic demyelination syndrome (ODS) remains a significant risk associated with overcorrection, even with the use of desmopressin (DDAVP).
- The evidence remains inconclusive regarding the superiority of proactive versus reactive DDAVP administration in preventing overcorrection.
- Further research is needed to determine optimal DDAVP dosage and timing, considering individual patient risk factors for
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026