Low sodium in the blood (hyponatremia) can be a complex condition to manage effectively in a hospital setting. This comprehensive guide provides a clear, step-by-step protocol for the accurate diagnosis and treatment of hyponatremia. We will delve into the various types of hyponatremia, explain the factors influencing treatment selection, and outline the essential monitoring procedures to prevent potential complications. The focus is on providing cutting-edge, safe, and effective methods to optimize patient care in hyponatremia management. For more detailed guidelines, see these hyponatremia treatment guidelines.
Hyponatremia Hospital Protocol: A Step-by-Step Guide to Safe and Effective Treatment
Hyponatremia, defined as low sodium levels in the blood, presents a significant health concern, and this protocol offers guidance to manage it safely and effectively within a hospital setting for adult patients. Remember that each patient’s situation is unique, and thus these steps offer a foundation for individualized treatment plans. This guide focuses on evidence-based approaches to diagnosis, treatment, and monitoring.
Comprehensive Patient Assessment: Clinical Evaluation and Diagnostic Tests
A thorough patient assessment is paramount. This assessment serves as the foundation for an effective treatment plan. Understanding both the severity and underlying cause is essential.
Step 1: Determine the Severity of Hyponatremia. Measure serum sodium levels. The degree of hyponatremia determines the urgency and intensity of the intervention required. Mild hyponatremia (130-135 mEq/L) necessitates a different approach than severe cases (<120 mEq/L).
Step 2: Evaluate Fluid Balance. Determine the patient’s fluid status. Is the patient hypovolemic (dehydrated), euvolemic (normal fluid levels), or hypervolemic (excess fluid)? A physical examination, including assessment of skin turgor, mucous membranes, jugular venous pressure, and edema, is crucial.
Step 3: Identify The Underlying Cause. Investigate the etiology of the hyponatremia. Potential causes include medications (diuretics, SSRIs), kidney disease, heart failure, liver cirrhosis, syndrome of inappropriate antidiuretic hormone secretion (SIADH), adrenal insufficiency, and primary polydipsia. Obtain a detailed patient history, medication list, and relevant laboratory tests.
Treatment Strategies: A Tailored Approach
Treatment is highly individualized and dependent on the underlying cause, the severity of hyponatremia, the patient’s volume status (hypovolemic, euvolemic, or hypervolemic), and the presence of symptoms.
Hypovolemic Hyponatremia (Dehydration): This condition is characterized by both sodium and water loss. The primary management strategy involves replenishing both volume and sodium deficits with intravenous isotonic saline (0.9% NaCl). Close monitoring of serum sodium levels is essential to avoid overly rapid correction.
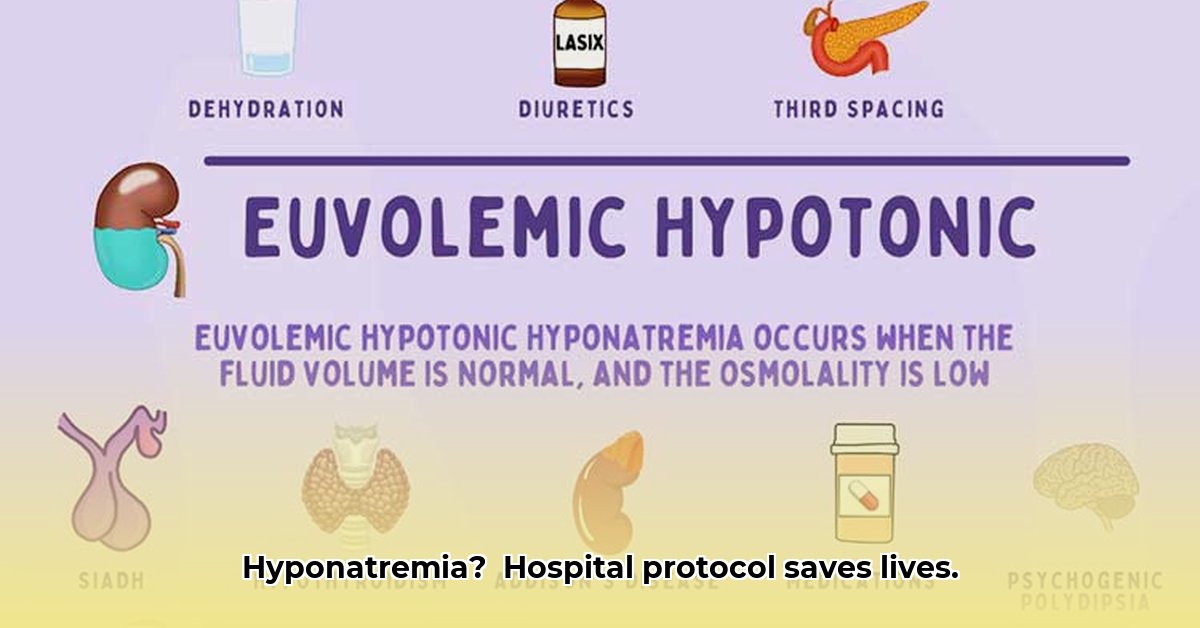
Euvolemic Hyponatremia (Normal Fluid Levels): In euvolemic hyponatremia, total body water is increased, leading to sodium dilution. Common causes include SIADH, hypothyroidism, and glucocorticoid deficiency. Fluid restriction is often the initial step in management, limiting fluid intake to less than 1 liter per day. In some cases, medications such as vaptans may be considered to promote water excretion.
Hypervolemic Hyponatremia (Fluid Overload): This condition is associated with excess fluid retention, diluting the sodium concentration. Common etiologies include congestive heart failure, cirrhosis, and nephrotic syndrome. Treatment focuses on addressing the underlying condition and promoting fluid excretion with diuretics (e.g., furosemide). Sodium restriction may also be beneficial.
Important Considerations:
- Rate of Correction: The rate of sodium correction is crucial. Rapid correction of chronic hyponatremia can lead to osmotic demyelination syndrome (ODS), a potentially devastating neurological complication. The recommended rate of correction is typically no more than 8-10 mEq/L per 24 hours.
- Symptomatic Hyponatremia: Patients with severe symptoms, such as seizures, altered mental status, or coma, may require more aggressive treatment with hypertonic saline (3% NaCl). However, even in these cases, careful monitoring and controlled correction rates are essential.
Here’s a table summarizing treatment approaches based on volume status:
| Volume Status | Primary Treatment | Secondary Considerations | Monitoring |
|---|---|---|---|
| Hypovolemic | Isotonic saline (0.9% NaCl) | Monitor for fluid overload | Serum sodium, urine output, vital signs |
| Euvolemic | Fluid restriction (≤ 1 liter/day) | Vaptans (tolvaptan, conivaptan) | Serum sodium, fluid balance, neurologic status |
| Hypervolemic | Diuretics (e.g., furosemide), Na restriction | Address underlying condition | Serum sodium, fluid balance, weight, electrolytes |
Monitoring and Prevention of Complications
Continuous monitoring is critical to ensure safe and effective management and to prevent complications such as ODS.
- Frequent Electrolyte Monitoring: Regularly monitor serum sodium levels, particularly during the initial phase of treatment.
- Neurological Assessments: Assess neurological function frequently for any signs of ODS (e.g., confusion, dysarthria, dysphagia, weakness).
- Fluid Balance Monitoring: Closely monitor fluid intake and output to guide fluid management.
Special Populations
Specific populations require extra consideration.
- Elderly: Elderly patients are more susceptible to hyponatremia and its complications.
- Patients with Chronic Conditions: Patients with heart failure, cirrhosis, or kidney disease require careful management to avoid exacerbating their underlying conditions.
The Evolving Landscape of Hyponatremia Management
Hyponatremia treatment is an evolving field. Ongoing research continues to refine risk assessment and personalize treatment strategies. Staying informed about the latest clinical guidelines and best practices ensures optimal patient outcomes.
How to Choose the Best Hyponatremia Treatment Based on Volume Status
Choosing the optimal treatment for hyponatremia (serum sodium <135 mEq/L) requires a systematic approach. The cornerstone of effective management is accurate assessment of the patient’s volume status. This section will explore this crucial diagnostic step.
Understanding the Clinical Signs of Volume Status
Accurate determination of volume status is paramount before initiating treatment.
- Hypovolemic Hyponatremia: Fluid and sodium are both depleted, with a relatively greater loss of sodium. Clinical signs include hypotension, orthostatic changes, tachycardia, dry mucous membranes, decreased skin turgor, and elevated BUN/creatinine ratio.
- Euvolemic Hyponatremia: Total body water is increased with normal sodium. Patients may appear clinically normal, although subtle signs of fluid overload (e.g., mild edema) may be present. Common causes include SIADH, psychogenic polydipsia, and hypothyroidism.
- Hypervolemic Hyponatremia: The body retains both sodium and water, but water retention predominates. Clinical features include edema (peripheral, pulmonary), jugular venous distension, and ascites. This is often associated with heart failure, cirrhosis, and nephrotic syndrome.
Diagnostic Workup: Beyond Volume Status
While volume status is critical, further information is needed for appropriate treatment.
- Serum Osmolality: This distinguishes true hyponatremia from pseudohyponatremia.
- Urine Sodium: A high urine sodium suggests renal sodium loss, while low levels point to extrarenal causes.
- Urine Osmolality: Helps differentiate SIADH from other causes of euvolemic hyponatremia.
- Clinical History: Obtain a complete medical history, including medications, pre-existing conditions, and recent symptoms.
- Medication Review: Certain drugs (e.g., diuretics, SSRIs, NSAIDs) can contribute to hyponatremia.
Treatment Strategies: Tailoring Care
Once volume status and other factors have been assessed, the appropriate treatment can be determined.
Hypovolemic Hyponatremia
The primary goal is to restore intravascular volume with isotonic saline (0.9% NaCl). Monitor serum sodium levels closely and avoid rapid correction. The rate of correction should not exceed 8-10 mEq/L per 24 hours.
Euvolemic Hyponatremia
Fluid restriction (typically 500-1000 mL/day) is the initial step; if ineffective, consider vaptans, but weigh the benefits against the risks.
Hypervolemic Hyponatremia
Focus on reducing fluid overload, use diuretics (loop diuretics are often preferred) and restrict dietary sodium.
Monitoring and Preventing Complications
Frequent monitoring is vital. The primary concern is osmotic demyelination syndrome (ODS).
- Monitor serum sodium levels every 4-6 hours during initial treatment.
- Assess neurological status regularly for signs of ODS.
Choosing the Best Treatment: A Simplified Approach
Use this evidence-based approach determined by volume status:
| Volume Status | Primary Treatment | Secondary Considerations |
|---|---|---|
| Hypovolemic | Isotonic saline resuscitation | Monitor for fluid overload, avoid rapid correction |
| Euvolemic | Fluid restriction | Vaptans (use with caution), treat underlying cause |
| Hypervolemic | Diuretics, sodium restriction | Address underlying cause (CHF |
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026