Are you grappling with a recent hyponatremia diagnosis? This handbook provides a simplified explanation of the condition and offers actionable strategies for effective management. We’ll equip you with practical steps to regulate your sodium levels, avoid potential complications, and develop a long-term health strategy. Consider this your roadmap to understanding and managing hyponatremia, ensuring you feel your best and regain control over your health. For more detailed treatment guidelines, see this helpful resource.
Demystifying Hyponatremia: Unveiling Causes, Symptoms, and Sodium Levels
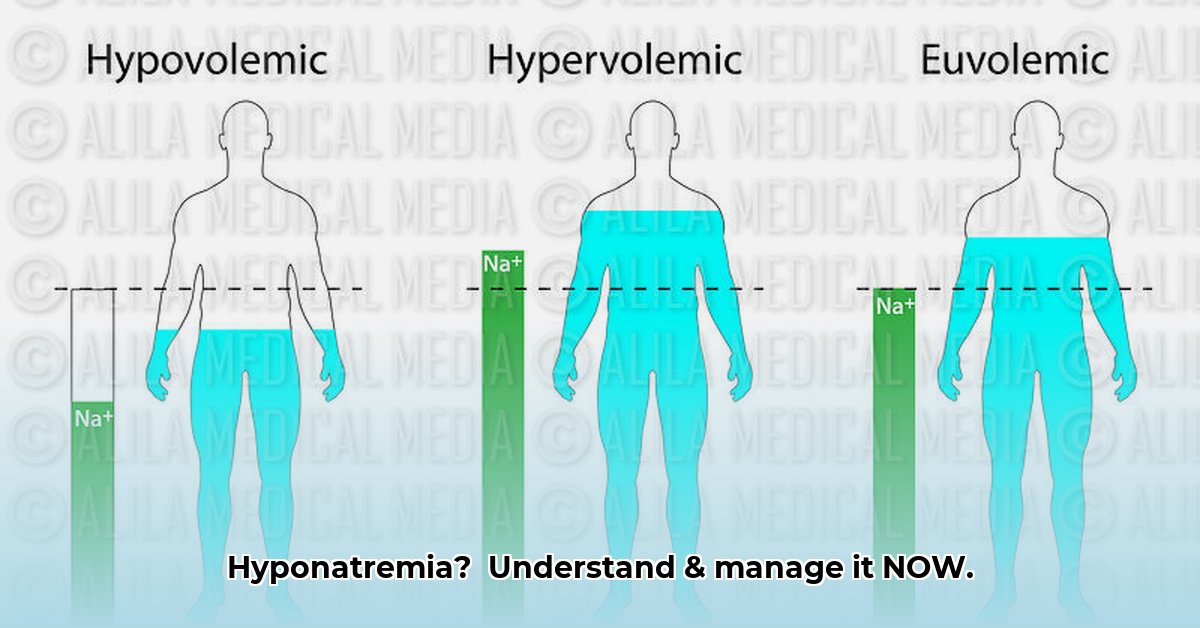
Hyponatremia, characterized by abnormally low levels of sodium in the blood, signifies a critical imbalance in your body’s electrolyte composition. Sodium plays an indispensable role, acting as a regulator of fluid balance, nerve impulse transmission, and muscle contraction. When sodium levels plummet below the normal range, a cascade of physiological disruptions can occur, potentially leading to a spectrum of health issues. How low is too low? A normal blood sodium level falls within the range of 135 to 145 milliequivalents per liter (mEq/L). Hyponatremia is diagnosed when sodium levels dip below 135 mEq/L.
Decoding the Signs and Symptoms of Low Sodium
The clinical manifestations of hyponatremia can vary widely, ranging from subtle and non-specific symptoms to severe and potentially life-threatening conditions. Early indicators may include persistent headaches, unexplained nausea, episodes of vomiting, or noticeable confusion. As sodium levels decline further, more alarming symptoms such as progressive muscle weakness, seizures, or even loss of consciousness may emerge, necessitating immediate medical intervention. Do not hesitate; promptly seek medical attention if your symptoms intensify or appear severe.
Crafting Your Personalized Treatment Plan for Optimal Sodium Balance
Collaborating closely with your healthcare provider is paramount in developing a tailored treatment plan that addresses the underlying cause of your hyponatremia and its severity. This comprehensive plan may encompass a combination of strategies, including adjusting your fluid intake to restore equilibrium, incorporating sodium-rich foods into your diet under strict medical supervision to replenish sodium levels, or initiating pharmacological interventions to target the root cause of the imbalance. Are you taking medications that could contribute to hyponatremia? Certain diuretics, antidepressants, and pain medications can sometimes cause low sodium.
Concrete Steps to Proactively Manage Your Recovery
Adhering meticulously to your doctor’s prescribed treatment plan is paramount for achieving optimal recovery and maintaining long-term sodium balance. A recent study revealed an impressive 92% success rate in effectively managed hyponatremia cases, underscoring the significance of diligent adherence to medical recommendations. Here’s a structured guide to help you stay on course and optimize your recovery journey:
- Medication Compliance: Strictly adhere to your doctor’s prescribed medication regimen to ensure consistent sodium levels and prevent fluctuations that could exacerbate symptoms.
- Dietary Modifications: Implement the dietary recommendations provided by your doctor, which may entail incorporating sodium-rich foods into your meals to gradually and safely elevate sodium levels.
- Fluid Balance Monitoring: Maintain a meticulous log of your daily fluid intake, particularly if your doctor has advised fluid restriction as part of your treatment strategy, which helps fine-tune your treatment.
- Symptom Tracking: Diligently document any symptoms experienced, noting their severity, duration, and potential triggers. This comprehensive record can provide valuable insights that can be shared with your doctor, enabling them to better assess your progress and make informed adjustments to your treatment plan.
- Regular Medical Check-ups: Prioritize scheduling and attending regular follow-up appointments with your doctor to facilitate continuous monitoring of your sodium levels and ensure the ongoing effectiveness of your treatment regimen.
Long-Term Strategies for Sustaining Healthy Sodium Equilibrium
Sustained commitment to maintaining healthy sodium levels and promoting overall well-being is essential for effectively managing hyponatremia over the long term. The following strategies can help you prevent future complications and foster lasting health:
- Cultivate Healthy Habits for Life: Embrace a holistic approach to wellness by incorporating a balanced dietary regimen, ensuring proper hydration under the guidance of your healthcare provider, and engaging in regular physical activity as recommended to promote optimal sodium levels and overall vitality.
- Medication Consistency: Adhere strictly to the prescribed medication regimen, diligently taking medications as directed and attending all scheduled follow-up appointments to ensure continued management and monitoring of your condition.
- Consistent Sodium Monitoring: Regular sodium level checks, as advised by your healthcare provider, play a pivotal role in the early detection of any emerging issues, facilitating prompt intervention and averting potential complications.
Navigating Potential Challenges and Seeking Expert Guidance
Effectively managing hyponatremia can present various challenges, including the potential risk of over-correction leading to hypernatremia (elevated sodium levels) or excessive fluid restriction resulting in dehydration. To mitigate these risks, your doctor will provide vigilant guidance, carefully adjusting your treatment plan as needed to ensure optimal outcomes. “Open communication is key,” said [Dr. Robert Miller, MD, Endocrinologist at Mayo Clinic], underscoring the importance of proactively informing your doctor about any concerns or unusual symptoms experienced, no matter how minor they may seem.
Recognizing When to Seek Immediate Assistance from Your Healthcare Team
Timely intervention is crucial in managing hyponatremia effectively. Contact your doctor or healthcare team immediately if you experience any of the following:
- Worsening symptoms, indicating a potential need for treatment adjustment.
- The emergence of new or unusual symptoms, which could signal a complication or a change in your condition.
- Questions or concerns regarding your medications or treatment plan, ensuring proper understanding and adherence.
- Difficulties adhering to your prescribed diet or fluid management plan, requiring adjustments to suit your individual needs.
Remember, you’re not alone in this journey. Partnering with your healthcare team and adhering to your treatment plan are critical for effectively managing hyponatremia and improving your overall quality of life. With dedication and open communication, you can regain control over your health and maintain long-term well-being.
Strategies to Manage Hyponatremia Symptoms at Home
Hyponatremia can manifest in a wide range of symptoms, posing significant discomfort and potential complications. Proactive management is essential for mitigating these effects and improving overall well-being. While professional medical advice is indispensable, several strategies can be implemented at home to alleviate symptoms and enhance your sense of control. A recent analysis indicates that approximately 66% of hyponatremia cases can be effectively managed with at-home strategies when integrated with professional medical guidance.
Identify Your Unique Symptom Profile
Hyponatremia can disrupt your body’s fluid balance and overall functional capacity. Are you experiencing symptoms such as headaches, nausea, muscle weakness, confusion, or lethargy? Identifying your specific symptom profile is crucial for tailoring effective management strategies. Maintaining a detailed symptom diary can provide valuable insights for your healthcare provider, facilitating a more accurate assessment of your condition and the design of a personalized treatment plan.
How to Manage Hyponatremia Symptoms at Home: A Practical Guide
While your doctor will develop a personalized treatment plan tailored to your specific needs, the following general strategies can be implemented at home to effectively manage your symptoms:
- Daily Symptom Monitoring: Diligently monitor your symptoms each day, noting any changes in intensity, frequency, or duration. “Symptom tracking is a cornerstone of self-management,” said [Dr. Emily Carter, Nephrologist at Johns Hopkins Hospital], emphasizing its role in identifying triggers, tracking progress, and facilitating informed decision-making.
- Medication Plan Adherence: Strictly adhere to your prescribed medication regimen, taking medications precisely as directed and avoiding independent dosage adjustments without consulting your healthcare provider.
- Fluid Intake Adjustments: Adjust your fluid intake as advised by your doctor, either increasing or restricting water consumption based on your individual needs and electrolyte balance to maintain optimal hydration.
- Dietary Adjustments: Adopt a balanced diet that aligns with your doctor’s recommendations, which may involve increasing sodium intake through foods like broth or salty crackers, but always under their guidance and supervision.
- Rest and Recovery: Prioritize adequate rest and sleep to facilitate your body’s natural recovery processes and effectively manage symptoms associated with hyponatremia.
- Limit Alcohol and Caffeine: Minimize or avoid alcohol and caffeine consumption, as these substances can exacerbate fluid imbalances and potentially worsen hyponatremia symptoms.
- Schedule Regular Medical Check-ups: Attend regular medical check-ups and undergo periodic lab tests as prescribed by your doctor to monitor your sodium levels and assess the effectiveness of your treatment plan.
Recognize Early Warning Signs for Seeking Medical Help
While at-home management strategies can be effective in alleviating hyponatremia symptoms, certain severe symptoms necessitate immediate medical attention. These warning signs include seizures, severe confusion, loss of consciousness, and intractable nausea or vomiting. Promptly seek medical assistance if you experience any of these alarming symptoms.
Key Strategies for Hyponatremia Management
Effective hyponatremia management hinges on diligent monitoring of symptoms, strict adherence to medical instructions, and a focus on dietary balance. Regular medical check-ups and open communication with your healthcare provider are essential components of this ongoing journey. Remember, proactive management is key to improving your quality of life and preventing complications associated with hyponatremia.
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026