Hyponatremia, a condition characterized by low serum sodium levels, presents a significant clinical challenge requiring careful management. While effective treatment is crucial, guidelines remain a subject of ongoing debate and refinement. For more on acute hyponatremia treatment, see this resource. This article offers a detailed exploration of the current consensus, controversies, and the latest research surrounding hyponatremia management, providing valuable insights for clinicians and healthcare professionals.
The Delicate Balance: Managing Low Sodium and Safeguarding the Brain
Severe hyponatremia is a critical medical condition with potentially serious health implications. The primary goal of treatment is a gradual and controlled increase in serum sodium levels. Rapid correction poses a substantial risk of osmotic demyelination syndrome (ODS), a devastating neurological disorder. Consequently, ongoing research efforts are heavily focused on minimizing this risk and ensuring brain safety during hyponatremia treatment. What are the specific mechanisms by which slow correction prevents ODS?
- Gradual sodium level correction is essential to prevent the potentially irreversible neurological damage associated with ODS.
- The optimal speed of correction must be carefully tailored to the individual patient, considering the severity, duration, and underlying cause of hyponatremia.
- Effective treatment strategies involve a multifaceted approach, including fluid management, judicious administration of hypertonic saline, and identification and treatment of the underlying cause of the sodium imbalance.
Navigating the Treatment Landscape: Balancing Correction Speed and Patient Safety
Historically, the cornerstone of hyponatremia treatment has been the avoidance of rapid increases in serum sodium levels, particularly in patients with chronic hyponatremia. Many sources emphasize the potential for ODS when correcting very low sodium levels (≤115 mmol/L) too quickly. Clinicians often rely on predictive formulas, such as the Adrogue-Madias equation, to guide their treatment approach. However, these formulas have limitations and may not accurately predict patient response in all cases. What are the known limitations of existing predictive formulas in hyponatremia treatment?
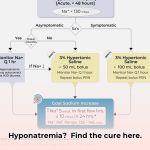
Recent large-scale studies have challenged the traditional emphasis on extreme caution, suggesting that the risk of ODS may be overstated, particularly in cases of acute hyponatremia (a new onset of low sodium). This evolving perspective has led to a shift in the treatment paradigm, with some experts suggesting that faster correction may be safer in certain acute scenarios. However, the majority of experts continue to advocate for a cautious approach until further research definitively clarifies the optimal correction speed, always prioritizing patient safety and minimizing the risk of neurological complications.
Comprehensive Patient Assessment: The Key to Personalized Hyponatremia Treatment
The duration of hyponatremia (acute vs. chronic) is a critical factor in determining the appropriate treatment strategy. A sudden drop in serum sodium levels may justify a slightly faster correction rate compared to a patient with long-standing, chronic hyponatremia. Accurate diagnosis is paramount, requiring a thorough medical history, physical examination, and laboratory evaluation to identify the underlying cause of hyponatremia. Clinicians must also carefully consider the patient’s fluid balance, symptoms, and concurrent medical conditions when selecting the most appropriate saline solution (hypertonic vs. isotonic), emphasizing the need for personalized treatment plans based on a comprehensive patient assessment.
Tailored Treatment Strategies: A Patient-Centric Approach
Individualized treatment planning is essential for the effective management of hyponatremia. The following table outlines actionable steps for different stakeholders involved in hyponatremia care:
| Stakeholder | Short-Term Actions (0-1 year) | Long-Term Actions (3-5 years) |
|---|---|---|
| Clinicians | Adhere to current evidence-based guidelines; meticulously assess the duration, severity, and underlying cause of hyponatremia; utilize predictive formulas judiciously, recognizing their limitations; rigorously monitor serum sodium levels and neurological status; and individualize treatment based on patient-specific factors, such as age, medical history, concurrent conditions, and response to therapy. | Actively participate in clinical research to refine correction rate recommendations; develop and implement improved diagnostic tools to accurately differentiate between acute and chronic hyponatremia; contribute to the development of evidence-based updates in clinical practice guidelines. |
| Researchers | Conduct large-scale, well-designed clinical trials to validate existing treatment protocols and identify optimal correction rates; investigate the limitations of predictive formulas and develop more accurate models; explore novel therapeutic interventions, such as selective sodium channel modulators and vasopressin receptor antagonists; and refine diagnostic imaging techniques, such as advanced MRI, to predict and detect early signs of ODS risk. | Develop more accurate and personalized predictive models incorporating advanced biomarkers and genetic information; explore novel treatments targeting the underlying pathophysiology of hyponatremia, including gene therapy and personalized medicine approaches; and investigate the role of inflammation and oxidative stress in the pathogenesis of hyponatremia-induced brain injury. |
| Regulatory Bodies | Review existing guidelines and update them based on emerging evidence; strengthen safety protocols and oversight mechanisms to minimize the risk of ODS; increase awareness and education among healthcare providers through evidence-based educational programs and professional development initiatives; and promote the standardization of treatment protocols to improve patient safety and outcomes. | Improve the monitoring and regulation of hyponatremia research; implement standardized reporting metrics and adverse event tracking systems; establish interdisciplinary task forces comprising clinicians, researchers, and patient advocates to address knowledge gaps and promote collaborative research efforts. |
| Patients & Caregivers | Seek prompt medical care for symptoms suggestive of hyponatremia; actively participate in the monitoring and treatment process; adhere to prescribed medication regimens and lifestyle modifications, such as fluid restriction; and maintain open communication with healthcare providers to address concerns and report any adverse effects promptly. | Advocate for increased research funding and the development of better treatment options; support patient advocacy groups dedicated to hyponatremia awareness and education; participate in clinical trials to advance knowledge and improve outcomes; and foster partnerships between patients, clinicians, and researchers to accelerate the translation of research findings into clinical practice. |
The Future of Hyponatremia Management: Research and Innovation
Given the conflicting messages and ongoing uncertainties surrounding hyponatremia treatment, a rigorous, evidence-based approach is essential. More well-designed, prospective studies are needed to confirm optimal correction methods, identify risk factors for ODS, and address remaining uncertainties. Collaboration among clinicians, researchers, and regulatory bodies is crucial for developing improved guidelines that enhance patient outcomes and minimize the risk of complications. The ultimate goal is to achieve the ideal balance—avoiding both too-slow and too-fast corrections—to optimize patient safety and neurological outcomes. Could artificial intelligence (AI) and machine learning algorithms play a role in predicting optimal correction rates and personalizing hyponatremia treatment in the future?
Safe Correction of Severe Hyponatremia in Adults: An Evidence-Based Approach
Severe hyponatremia requires a cautious and gradual correction strategy to prevent potentially devastating neurological complications. The optimal correction speed depends on the severity of hyponatremia, the presence of symptoms, and the patient’s overall clinical condition. Treatment typically involves a combination of fluid restriction, hypertonic saline administration, and frequent monitoring of serum sodium levels. Individualized treatment plans are essential, considering the underlying cause of hyponatremia and the patient’s response to therapy.
Addressing the Challenges of Severe Hyponatremia
Hyponatremia, characterized by abnormally low blood sodium levels, presents unique challenges in adult patients. Severe cases require particularly careful management due to the risk of rapid changes leading to osmotic demyelination syndrome (ODS), a potentially irreversible form of brain damage. Adhering to evidence-based principles is crucial for how to safely correct severe adult hyponatremia based on latest research.
The Importance of Gradual Correction
The principle of gradual correction is paramount in how to safely correct severe adult hyponatremia based on latest research. Serum sodium levels must be increased slowly and deliberately to minimize the risk of ODS. The rate of correction should be individualized based on the severity of hyponatremia, the presence of symptoms, and the patient’s overall clinical presentation. Symptomatic individuals may require slightly faster correction, but rapid correction should generally be avoided.
Multifaceted Treatment Strategies
Effective treatment strategies for severe hyponatremia are multifaceted and tailored to the individual patient, commonly involving:
- Fluid Restriction: Limiting fluid intake helps the body restore sodium balance by reducing the dilutional effect.
- Hypertonic Saline: Intravenous administration of hypertonic saline may be necessary in severe cases to rapidly increase serum sodium levels.
- Careful Monitoring: Frequent blood tests are essential to monitor serum sodium levels and adjust the treatment plan accordingly.
- Addressing Underlying Causes: Identifying and treating the underlying cause of hyponatremia is critical for long-term management and prevention of recurrence.
Balancing Speed and Safety
Balancing the need for effective correction with the risks of rapid correction is a significant challenge in the management of severe hyponatremia. The optimal correction rate is often debated, emphasizing the importance of individualized treatment plans and continuous monitoring. Regular assessments of serum sodium levels guide adjustments to the treatment strategy. Clinicians must remain adaptable and responsive to the patient’s clinical response, emphasizing ongoing assessment and refinement of the treatment plan.
Refining Hyponatremia Treatment through Research
Ongoing research continues to explore refined treatment strategies and predictive models for assessing ODS risk. Advances in
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026