Chronic hyponatremia, marked by persistently low sodium levels in the blood, necessitates careful and consistent management strategies that extend beyond simply increasing salt intake. For more information on symptoms, see this helpful guide on chronic hyponatremia symptoms. The cornerstone of effective management lies in pinpointing the underlying cause of the low sodium levels. This detailed guide offers clear, actionable steps for clinicians and patients alike, designed to navigate the intricacies of chronic hyponatremia.
Diagnosing Low Sodium: Unveiling the Root Cause Through Key Diagnostic Criteria
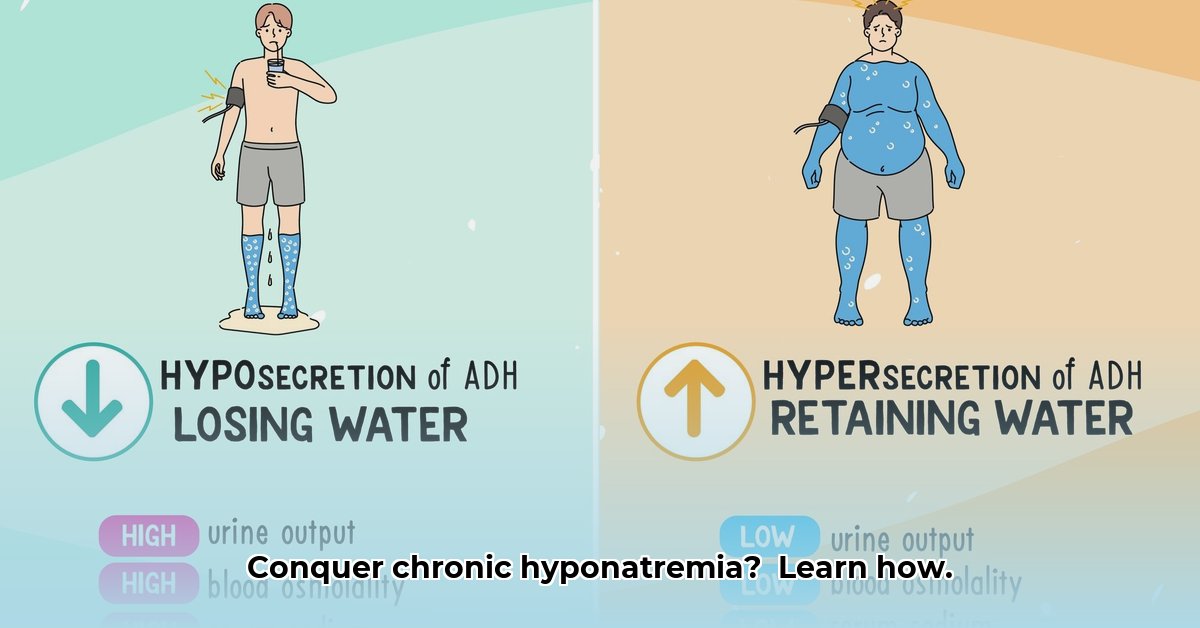
The initial and critical step in managing chronic hyponatremia is to accurately diagnose its underlying cause. This involves a comprehensive evaluation utilizing a range of diagnostic tools to accurately identify the type of chronic hyponatremia. Blood tests are paramount for assessing sodium levels and hydration status. Urine tests are essential to determine whether the body is losing excessive sodium or retaining too much water. In select cases, imaging studies such as an MRI scan may be warranted for a more detailed internal assessment. The primary goal is to determine whether the patient is hypovolemic (dehydrated), euvolemic (normally hydrated), or hypervolemic (overhydrated).
Treatment Strategies: A Gradual Approach to Sodium Correction
Managing chronic hyponatremia demands a deliberate and gradual approach to minimize the risk of potential complications, notably osmotic demyelination syndrome (ODS), a severe neurological condition that can arise from a rapid increase in sodium levels. Patience and vigilant monitoring are paramount throughout the treatment process.
Step 1: Fluid Balance Management
Adjusting fluid intake is frequently the initial step. When the body is retaining excessive water, a reduction in fluid consumption may be advised. Conversely, dehydration may necessitate an increase in fluid intake. Recommendations should be meticulously tailored to individual needs, striving to maintain optimal fluid balance.
Step 2: Dietary Modifications
Adjusting the diet to augment sodium intake through food or supplements may be essential. However, this must be undertaken under strict medical supervision, as excessive sodium intake can be detrimental.
Step 3: Medication Assessment
Certain medications can contribute to low sodium levels. A thorough review of the patient’s current medication regimen can identify potential culprits, leading to dosage adjustments, medication switches, or the discontinuation of specific drugs. The overarching goal is to optimize medication use without negatively impacting overall health.
Step 4: Addressing Underlying Conditions
Low sodium levels may be symptomatic of underlying health conditions such as heart failure or kidney disease. Effectively managing the primary health problem is crucial for the long-term management of hyponatremia.
Monitoring and Prevention: Long-Term Strategies for Sustained Well-Being
Regular follow-up appointments and blood tests are vital for monitoring sodium levels and assessing the effectiveness of the treatment plan. Early identification of any issues allows for prompt adjustments, mitigating the risk of complications. Long-term management is essential for sustained well-being. Detecting issues early allows for timely adjustments, reducing the chances of complications.
Potential Complications and Their Management
While the objective is a seamless treatment process, potential complications may arise. The table below summarizes common complications and their respective management strategies:
| Complication | Clinical Significance | Management Strategies |
|---|---|---|
| Osmotic Demyelination Syndrome (ODS) | Severe neurological damage resulting from a rapid increase in sodium levels. | Slow, gradual sodium correction; meticulous monitoring; supportive care. |
| Seizures | Sudden, uncontrolled electrical activity in the brain, potentially triggered by severe hyponatremia. | Immediate medical intervention; intravenous (IV) sodium administration; supportive care. |
| Neurological Symptoms | Manifestations such as headaches, nausea, vomiting, confusion, dizziness, weakness, and more. | Treatment strategies individualized to the severity of symptoms, potentially including hospitalization and IV fluids. |
Important Note: The information provided in this guide is intended for educational purposes only and should not be construed as a substitute for professional medical advice. Individuals should consult with a qualified healthcare provider to develop a personalized, safe, and effective treatment plan tailored to their specific health needs. The management of chronic hyponatremia should be a collaborative effort between the patient and their physician.
Tailoring Hyponatremia Treatment Based on Volume Status: A Personalized Approach
Accurate assessment of volume status (hypervolemic, hypovolemic, euvolemic) is critical for effective hyponatremia treatment, as treatment strategies vary significantly based on the patient’s fluid balance. Plasma osmolality and urinary sodium levels assist in diagnosis and targeted therapy. Gradual sodium correction is essential to prevent ODS.
The Importance of Volume Status Assessment
Prior to initiating any treatment, accurately determining the patient’s volume status is paramount, as this classification guides the selection of appropriate management strategies. Volume status is categorized into three types:
- Hypervolemic: Characterized by fluid overload, often observed in conditions such as heart failure or liver cirrhosis, where the body retains excess fluid.
- Hypovolemic: Characterized by fluid depletion, commonly caused by dehydration or diuretic use.
- Euvolemic: Characterized by normal fluid volume, most commonly associated with conditions like syndrome of inappropriate antidiuretic hormone (SIADH).
Refining Diagnosis: Advanced Diagnostic Tools
Further investigations are required to refine the diagnosis.
- Plasma osmolality: Measures the concentration of dissolved particles in the blood. Low osmolality suggests a dilution problem.
- Urinary sodium: Measures the amount of sodium excreted in urine. High levels often indicate renal sodium loss.
Treatment Strategies: A Tailored Approach
Treatment approaches vary based on volume status:
1. Hypervolemic Hyponatremia:
- Fluid restriction: The primary intervention, aiming to reduce excess fluid.
- Diuretics: Employed cautiously, with close monitoring, as they can worsen sodium deficit if mismanaged.
2. Hypovolemic Hyponatremia:
- Fluid resuscitation: Involves replenishing lost fluids with isotonic saline solutions.
- Address underlying cause: Manage conditions like diarrhea or vomiting, or adjust medication regimens.
3. Euvolemic Hyponatremia (e.g., SIADH):
- Fluid restriction: Often the initial step.
- Vaptans: Medications that block vasopressin (ADH) action and increase free water excretion, which is used under close clinical observation.
Preventing Complications: Gradual Correction
Rapid sodium correction can lead to severe consequences, including ODS. Therefore, gradual correction, typically at a rate of 8-10 mmol/L per day, is essential.
Continuous Assessment: Ongoing Monitoring
Regular monitoring of serum sodium levels, fluid balance, and clinical symptoms is crucial. Adjustments may be needed based on the patient’s response to treatment.
Managing Hyponatremia in Geriatric Patients: A Specialized Approach
Hyponatremia is more prevalent among older adults owing to age-related physiological changes, polypharmacy, and underlying health conditions. Chronic hyponatremia often presents subtly, delaying diagnosis and treatment and increasing the risk of falls, cognitive decline, and fractures. Effective management requires careful consideration of hydration, sodium intake, and medication interactions.
Understanding the Unique Challenges
Older adults exhibit impaired fluid regulation, commonly take multiple medications that can affect sodium levels, and frequently have underlying conditions like heart failure or kidney disease that complicate hyponatremia management.
Step-by-Step: Diagnosing Hyponatremia
Accurate diagnosis is essential:
- Comprehensive History and Physical Exam: Assess symptoms, medications, and fluid intake and note any falls or cognitive changes.
- Laboratory Evaluations: Use blood tests to measure serum sodium levels and osmolality. Urine tests help determine the cause.
- Volume Status Evaluation: Determine if the patient is hypovolemic, euvolemic, or hypervolemic to guide treatment.
Treatment Strategies: Individualized Geriatric Care
Treatment aligns with the severity and underlying cause:
- Mild Hyponatremia: Careful monitoring and adjustments to fluid and sodium intake may suffice. An individualized approach is vital.
- Moderate to Severe Hyponatremia: More aggressive management, including intravenous fluids, medications, or dietary adjustments, may be needed to restore sodium levels slowly and safely.
Optimizing Medication Regimens
Medications, including diuretics and antidepressants, can contribute to hyponatremia. A thorough medication review is essential in managing hyponatremia in the elderly.
Long-Term Management: Ongoing Monitoring
Regular monitoring of serum sodium levels is crucial for early detection of recurrence or fluctuations.
Potential Causes of Hyponatremia in Geriatric Patients
| Cause Category | Specific Example | Contributing Factors |
|---|---|---|
| Medications | Diuretics | Increased sodium excretion, fluid loss |
| Medical Conditions | Heart Failure | Fluid retention, decreased kidney function |
| Hormonal Imbalances | Hypothyroidism | Impaired water excretion |
| Lifestyle/Dietary Factors | Low Sodium Diet | Insufficient sodium intake |
| Age-Related Changes | Reduced Kidney Function | Decreased ability to regulate fluid and electrolyte balance |
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026