Have you ever considered how a seemingly simple electrolyte imbalance like low sodium in your blood could profoundly impact your mental well-being? This article delves into the intricate relationship between hyponatremia (low sodium levels) and alterations in mental state. For more information on hyponatremia ICD-10 codes, see this helpful resource: ICD-10 Codes. We’ll dissect the various classifications of hyponatremia, elucidate their mechanisms of action within the brain, and furnish actionable guidance for effective management. This review also encompasses early detection strategies, preventative measures, and forward-looking approaches, empowering you with insights to confidently navigate this condition.
Mental Status Changes and Cognitive Impairment in Hyponatremia
Hyponatremia, clinically defined as a serum sodium concentration below the normal range, exerts significant influence over optimal brain function. Sodium plays a pivotal role in maintaining the delicate fluid balance within brain cells, facilitating proper nerve impulse transmission and overall neurological stability. When sodium levels decline, an osmotic gradient is created, causing water to shift into brain cells, leading to cellular swelling and subsequent disruption of normal neuronal activity. This cerebral edema manifests in a spectrum of mental status changes, ranging from subtle cognitive deficits to severe neurological sequelae, including seizures and coma; the severity and rapidity of onset dictate the clinical presentation. Are healthcare providers adequately equipped to identify and manage subtle cognitive deficits associated with sodium imbalances, particularly in vulnerable patient populations?
The Diverse Range of Hyponatremia Symptoms: Decoding the Signals
The clinical manifestations of hyponatremia-induced mental status changes are notably heterogeneous, spanning a continuum from subtle cognitive impairments to overt neurological dysfunction. Individuals may initially experience nonspecific symptoms such as:
- General malaise
- Headache
- Nausea
As hyponatremia progresses, more pronounced neurological symptoms may emerge, including:
- Confusion
- Lethargy
- Disorientation
- Agitation
In severe cases, patients may exhibit:
- Seizures
- Coma
- Permanent brain damage
The underlying etiology and rate of sodium decline are critical determinants of symptom severity; rapid-onset hyponatremia is often associated with more pronounced neurological deficits due to the brain’s limited capacity to adapt to acute osmotic shifts. Moreover, preexisting neurological or psychiatric conditions may confound the clinical picture, complicating diagnostic efforts. Can clinicians reliably distinguish between psychiatric manifestations directly attributable to hyponatremia and those arising from underlying psychiatric disorders?
Unveiling the Causes of Low Sodium: Identifying the Culprits
Hyponatremia can arise from a multitude of underlying causes, broadly categorized as follows:
- Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH): Characterized by excessive secretion of antidiuretic hormone (ADH), leading to impaired water excretion and dilutional hyponatremia.
- Psychogenic Polydipsia: Excessive water intake, often observed in individuals with psychiatric disorders, overwhelms the kidneys’ excretory capacity, resulting in hyponatremia.
- Medications: Certain medications, including diuretics, antidepressants (SSRIs, SNRIs), and anticonvulsants, can disrupt sodium balance, either by promoting ADH release or impairing renal sodium reabsorption.
- Medical Conditions: Underlying medical conditions such as heart failure, kidney disease, and liver cirrhosis can compromise sodium regulation, predisposing individuals to hyponatremia.
- Hormonal Imbalances: Adrenal insufficiency and hypothyroidism can disrupt electrolyte balance, increasing the risk of hyponatremia.
Given the diverse range of potential etiologies, a comprehensive evaluation is imperative to identify the underlying cause and guide appropriate management strategies. Are patients adequately informed about the potential risks of hyponatremia associated with commonly prescribed medications?
Diagnosing and Treating Low Sodium: Navigating the Complexities
The diagnosis of hyponatremia is typically established through laboratory assessment of serum sodium levels; however, determining the underlying cause requires a more nuanced and systematic approach. Diagnostic evaluation may include:
- Detailed medical history and physical examination
- Assessment of fluid balance and medication review
- Measurement of urine electrolytes and osmolality
- Hormonal studies
The treatment of hyponatremia is tailored to the underlying cause, severity, and rate of onset. Management strategies may include:
- Fluid restriction
- Sodium supplementation
- Diuretics
- Vasopressin receptor antagonists (vaptans)
- Treatment of underlying medical conditions.
Rapid correction of chronic hyponatremia carries the risk of osmotic demyelination syndrome (ODS), a potentially devastating neurological complication characterized by irreversible brain damage. Therefore, a slow, controlled approach to sodium correction is generally preferred, with close monitoring of neurological status and serum electrolyte levels. How can healthcare providers optimize their assessment of hyponatremia etiology and severity while employing treatment strategies that minimize the risk of complications?
Identifying High-Risk Groups: Understanding Vulnerability Factors
Certain populations are disproportionately susceptible to hyponatremia, including:
- Elderly Individuals: Age-related decline in renal function, impaired thirst mechanisms, and increased prevalence of comorbidities and polypharmacy contribute to hyponatremia risk.
- Individuals with Psychiatric Disorders: Psychogenic polydipsia, medication side effects, and underlying medical conditions increase the likelihood of hyponatremia in this population.
- Patients with Chronic Medical Conditions: Heart failure, kidney disease, liver cirrhosis, and adrenal insufficiency predispose individuals to electrolyte imbalances, including hyponatremia.
- Athletes: Endurance athletes who engage in prolonged, strenuous exercise and consume excessive amounts of hypotonic fluids are at risk of exercise-associated hyponatremia.
Proactive identification and monitoring of high-risk groups are essential for early detection and prevention of hyponatremia-related complications. What preventative strategies can be implemented to effectively mitigate the risk of hyponatremia in individuals with pre-existing conditions?
The Power of Early Detection: A Proactive Approach for Better Outcomes
Early detection of hyponatremia is paramount to avert serious neurological sequelae. Regular monitoring of serum sodium levels is recommended for individuals at increased risk, particularly those with underlying medical conditions, psychiatric disorders, or those taking medications known to affect sodium balance. Patients and caregivers should be educated about the signs and symptoms of hyponatremia, empowering them to seek prompt medical attention when warranted. Can widespread public awareness campaigns improve early detection rates and ultimately enhance patient outcomes?
Collaborative Strategies for Healthcare Providers and Patients: A United Front
Effective management of hyponatremia necessitates a collaborative approach involving healthcare providers, patients, and caregivers.
For Healthcare Professionals:
- Routinely assess serum sodium levels in at-risk patients.
- Consider hyponatremia in the differential diagnosis of unexplained mental status changes.
- Educate patients about risk factors, symptoms, and preventative measures.
- Employ slow, controlled methods for correcting sodium deficits.
- Collaborate with specialists (nephrologists, endocrinologists, psychiatrists) as needed.
For Patients:
- Understand your individual risk factors (age, medical conditions, medications).
- Promptly report any new or worsening symptoms to your healthcare provider.
- Adhere to prescribed medication regimens and fluid management strategies.
- Maintain open communication with your healthcare team.
Unanswered Questions and Future Research Directions: Charting New Territories
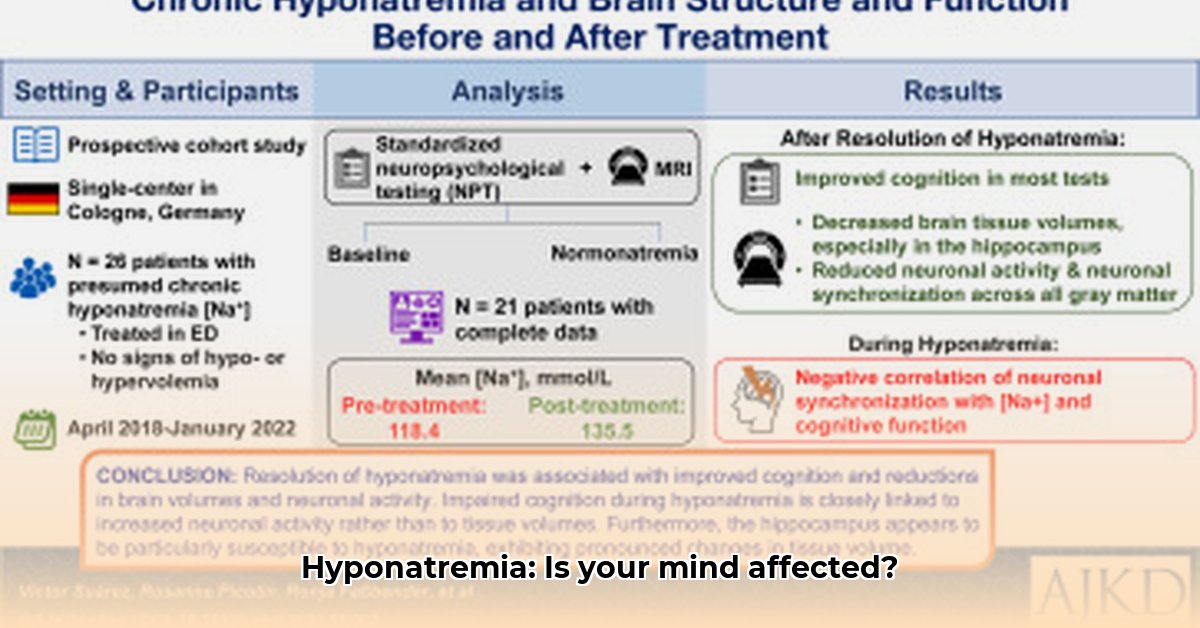
While considerable progress has been made in our understanding of hyponatremia and its impact on mental status, several questions remain unanswered. Further research is needed to:
- Elucidate the precise mechanisms by which hyponatremia affects specific cognitive domains and psychiatric symptoms.
- Determine the long-term consequences of mild to moderate hyponatremia on brain structure and function.
- Develop more targeted and personalized treatment strategies for hyponatremia, minimizing the risk of complications.
- Evaluate the effectiveness of novel interventions for preventing and managing hyponatremia in high-risk populations.
Further investigation is essential to refine our understanding of hyponatremia and optimize care practices for individuals affected by this prevalent yet frequently overlooked condition. How can future investigation optimize care practices, treatment approaches, and improve the broader understanding of this often-overlooked condition?
How to Safely Manage Hyponatremia-Induced Psychiatric Symptoms
Key Takeaways:
- Hyponatremia, characterized by low serum sodium levels, is a common clinical entity that can significantly impact neurological and psychiatric function. Its symptoms often overlap with those of primary mental health disorders, posing diagnostic challenges.
- Psychotropic medications, particularly selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), are implicated in the pathogenesis of hyponatremia, underscoring the importance of vigilant monitoring in patients receiving these agents.
- The management of hyponatremia-induced psychiatric symptoms hinges on the acuity and severity of the condition, as well as the presence of underlying medical or psychiatric comorbidities.
- Rapid correction of chronic hyponatremia can precipitate osmotic demyelination syndrome (ODS), a potentially devastating neurological complication; therefore, gradual and controlled sodium repletion is paramount.
- Effective management of hyponatremia necessitates a multidisciplinary approach, involving psychiatrists, internists, and pharmacists, to ensure optimal patient outcomes and minimize the risk of adverse events.
Decoding the Problem: The Impact of Hyponatremia on Cognitive Status
Hyponatremia, defined as a serum sodium concentration below 135 mEq/L, exerts a profound influence on brain function and mental status. Sodium is a critical electrolyte that plays a vital role in maintaining cell volume, nerve impulse transmission,
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026