Are you experiencing issues with low sodium levels? Mild hyponatremia is a prevalent condition. Understanding it is crucial for maintaining optimal health. This guide provides a comprehensive overview, covering causes, diagnosis, and effective management strategies. We aim to equip you with the knowledge necessary for prevention and long-term well-being. For more on acute hyponatremia treatment, see this resource.
Mild Hyponatremia Management: A Detailed Guide
Mild hyponatremia, indicated by a lower-than-normal sodium level in your blood, requires attention. This guide clarifies the condition, its treatments, and preventive measures. Consider it your personal roadmap to understanding and addressing this subtle imbalance. Do you have the knowledge to fully understand hyponatremia, its causes, and its treatment?
Understanding Sodium Levels: Beyond Simple Salt Intake
Mild hyponatremia is present when blood sodium levels fall slightly below the normal range, typically between 130 and 135 mEq/L (milliequivalents per liter). While often asymptomatic, it’s essential to address it to prevent progression to severe hyponatremia, a more serious condition. Uncovering the underlying cause is the first step toward improved health and overall wellness.
Several factors contribute to low sodium levels. These range from excessive water intake to certain medications or underlying health conditions, such as kidney or heart problems. A clear understanding of these causes is vital for effective management and long-term well-being.
Diagnostic Process: Identifying the Root Cause
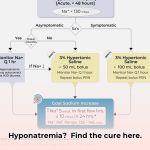
Diagnosing mild hyponatremia involves a comprehensive assessment of your hydration status and overall health. Your doctor will evaluate your medical history, current medications, and any symptoms you’re experiencing. They’ll also determine your fluid balance—whether you’re dehydrated, normally hydrated, or retaining excess fluid. This assessment guides the selection of the most appropriate treatment approach for positive outcomes.
Diagnostic tests are essential for proper evaluation. Your doctor will likely order blood tests to measure sodium levels, other electrolytes, and hormone levels. They may also inquire about your diet, recent illnesses, and lifestyle to gain a complete understanding of your health and identify the cause of the sodium deficiency.
Tailored Treatment Strategies: A Personalized Approach
Treatment for mild hyponatremia is not one-size-fits-all; it demands a personalized strategy. Your doctor will develop a tailored plan based on the underlying cause and severity of your low sodium, employing the most effective sodium management techniques. What specific treatments are appropriate for each scenario?
-
Hypovolemic Hyponatremia (Fluid Loss): In cases of fluid loss due to vomiting, diarrhea, or excessive sweating, treatment focuses on replenishing lost fluids with electrolyte solutions. This involves restoring lost sodium and other essential electrolytes with an optimal electrolyte balance, not just drinking plain water.
-
Euvolemic Hyponatremia (Excess Water): If excess water dilutes your body’s sodium, your doctor may recommend temporarily reducing fluid intake to allow your body to restore its sodium levels. This may involve drinking less water or other fluids to re-establish balance.
-
Hypervolemic Hyponatremia (Fluid Overload): This type often occurs with conditions like heart or kidney failure. Treatment addresses the underlying condition. Your physician may prescribe diuretics (water pills) to help your body eliminate excess fluid. Close medical supervision is crucial for safe and effective fluid regulation.
Important Note: Rapid correction of hyponatremia can lead to serious complications, such as central pontine myelinolysis (CPM), a potentially devastating condition. Your doctor will monitor your progress and adjust treatment accordingly, ensuring a gradual approach to restoring sodium levels.
Long-Term Prevention: Sustaining Sodium Balance
Sustained management of mild hyponatremia involves a long-term commitment to prevention. After initial treatment, the emphasis shifts to preventing future occurrences through lifestyle and dietary adjustments. What steps can you take to prevent hyponatremia in the long term?
-
Dietary Modifications: A balanced diet with adequate sodium is essential. Avoid drastic dietary changes without consulting your doctor. They can provide guidance on safe and effective adjustments to optimize dietary sodium intake.
-
Medication Review: Some medications can contribute to low sodium. Your doctor may suggest adjusting dosages or switching to alternatives to minimize this risk through careful medication review and necessary changes.
-
Lifestyle Adjustments: If an underlying health issue, such as heart or kidney disease, causes your low sodium, managing those conditions effectively is crucial for preventing future episodes of hyponatremia and improving overall health.
Continuous Monitoring: Maintaining Optimal Sodium Levels
Regular check-ups provide ongoing assessment and peace of mind. Your doctor will monitor your sodium levels, ensuring the effectiveness of your treatment plan and making adjustments as needed. Open communication is crucial for continuous improvement of care. Notify your doctor promptly if you experience any new or worsening symptoms.
Hyponatremia Subtypes and Treatment Strategies
| Hyponatremia Type | Description | Potential Treatments |
|---|---|---|
| Hypovolemic | Fluid loss (e.g., diarrhea, vomiting, excessive sweating) | IV fluids with electrolytes, oral rehydration solutions |
| Euvolemic | Excess water, impaired sodium excretion | Fluid restriction, medication adjustments (if necessary) |
| Hypervolemic | Fluid overload (e.g., heart failure, kidney failure) | Diuretics, treatment of underlying condition, sodium and fluid restriction if necessary |
Disclaimer: The information provided here is for educational purposes only and should not replace professional medical advice. Consult with your doctor for the diagnosis and treatment of any health concern. They are best suited to understand your individual situation and create a personalized plan. Research on hyponatremia is continually evolving. Stay informed and discuss any new developments with your physician.
Differentiating Hypovolemic from Euvolemic Hyponatremia Through Laboratory Markers
Key Insights:
- Hyponatremia is characterized by low sodium levels in the blood. It encompasses various subtypes, each necessitating a specific diagnostic and management strategy.
- Distinguishing between hypovolemic and euvolemic hyponatremia using laboratory markers is essential for effective treatment and appropriate interventions.
- Identifying the underlying cause of hyponatremia is essential for successful intervention and achieving optimal health outcomes.
- Careful monitoring of sodium levels is critical to prevent complications, such as osmotic demyelination syndrome (ODS), and maintain electrolyte balance.
- Treatment strategies are based on the specific type and severity of hyponatremia, requiring individualized and targeted care.
Deciphering Hyponatremia Subtypes
Let’s clarify the distinctions between different types of hyponatremia and their respective treatment strategies. In hypovolemic hyponatremia, fluid and sodium are lost, while euvolemic hyponatremia involves normal fluid levels but diluted sodium concentration. This distinction influences diagnostic and treatment approaches, emphasizing medical knowledge and individual patient considerations.
Decoding Laboratory Markers: Essential Diagnostic Indicators
Laboratory tests are essential diagnostic tools. Understanding the relationships between sodium, fluid volume, and urine concentration provides insight into the body’s fluid balance. Differentiating hypovolemic from euvolemic hyponatremia using lab markers requires careful interpretation of key values, integrating expertise with diagnostic data. What laboratory markers are vital for differentiating between these types of hyponatremia?
-
Serum Sodium Levels: This is the baseline measurement of sodium in your blood. Low levels are present in both conditions, requiring further investigation to determine the underlying cause.
-
Serum Osmolality Measurement: Serum osmolality measures the concentration of dissolved particles in the blood plasma. Low serum osmolality indicates dilutional hyponatremia, as seen in euvolemic hyponatremia.
-
Urine Osmolality and Sodium Analysis: In hypovolemic hyponatremia, the body attempts to conserve water, leading to high urine osmolality and low urine sodium concentration. Euvolemic hyponatremia often presents with high urine osmolality but a high urine sodium concentration, indicating that the kidneys are conserving sodium.
-
Assessing Other Electrolytes: Checking other electrolytes, such as blood urea nitrogen (BUN) and creatinine, aids in assessing kidney function and hydration status, providing further insights. An elevated BUN/creatinine ratio may suggest dehydration, indicative of hypovolemic hyponatremia.
Practical Diagnostic Application
A systematic approach can help you differentiate hypovolemic from euvolemic hyponatremia using lab markers. A combination of these factors will help to determine the final diagnosis and treatment plan based on the specific laboratory values in the patient.
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026