Low blood sodium, or hyponatremia, while seemingly minor, can escalate into a dangerous condition if it becomes severe. This guide aims to equip you with the necessary knowledge to recognize the signs, understand the causes, and, most importantly, know how to respond if you suspect someone is experiencing severe hyponatremia. We will demystify the symptoms, explain the diagnostic process, and guide you through the essential steps for seeking appropriate medical attention. For more detailed information on hyponatremia symptoms, see this helpful resource: Hyponatremia Symptoms. Additionally, we will explore strategies for preventing severe problems and effectively managing hyponatremia in the long term. Whether you are a patient, a caregiver, or a healthcare provider, this information is designed to empower you to take timely action and maintain optimal health.
Severe Hyponatremia Signs: Recognizing a Dangerous Imbalance
Hyponatremia signifies a state where the blood contains insufficient sodium. Normal sodium levels range from 135 to 145 milliequivalents per liter (mEq/L). When sodium levels fall below this range, particularly below 120 mEq/L, the risk of severe complications increases dramatically. While mild cases might not raise immediate alarm, severe hyponatremia can pose a life-threatening risk, emphasizing the importance of recognizing its warning signs. Envision it this way: a minor leak is manageable, but a burst pipe necessitates immediate intervention—severe hyponatremia mirrors the urgency of a burst pipe. Let’s familiarize ourselves with identifying the problem before it evolves into a critical emergency.
Understanding the Differences: Mild vs. Severe Hyponatremia
Not all instances of low sodium warrant concern. A mild case might only induce a headache, fatigue, or mild nausea. These symptoms can often be managed with simple lifestyle adjustments and close monitoring. Conversely, severe hyponatremia presents a starkly different scenario—a medical emergency demanding immediate intervention. The disparity lies in the intensity and rapid onset of symptoms. Minor cases often respond to simple adjustments, whereas severe cases necessitate urgent medical attention. The body relies on precise sodium levels for proper nerve and muscle function, and a significant imbalance can lead to serious consequences. What are the neurological symptoms to look out for?
Spotting the Red Flags: Symptoms of Severe Hyponatremia
Severe hyponatremia frequently manifests as neurological issues—affecting the brain and nervous system. These are the critical warning signs to observe:
- Seizures: Uncontrolled electrical disturbances in the brain, causing violent convulsions and loss of consciousness. This constitutes a life-threatening emergency. Seizures can present as brief staring spells, muscle jerking, or full-body convulsions.
- Coma: A state of deep, prolonged unconsciousness. A person in a coma is unresponsive to stimuli and requires immediate medical intervention. Coma can result from significant brain swelling due to severely low sodium levels.
- Confusion and Disorientation: Sudden difficulty concentrating, feelings of being lost, or exhibiting unusual behavior. These subtle changes can indicate a serious underlying issue. Individuals may not recognize their surroundings or understand simple instructions.
- Trouble Breathing (Respiratory Distress): Labored breathing, shallow breaths, or even cessation of breathing (respiratory arrest). This is a critical situation demanding immediate intervention. Hyponatremia can affect the muscles involved in breathing, leading to respiratory failure.
- Severe Nausea and Vomiting: Persistent and intense nausea and vomiting accompanied by other concerning symptoms. Excessive vomiting can further deplete sodium levels, exacerbating the condition.
- Intense Headache: A severe headache unresponsive to over-the-counter pain relievers. This could signal a more serious underlying condition. The headache may feel like a constant, dull pressure throughout the head.
- Muscle Weakness or Spasms: Significant muscle weakness or involuntary muscle spasms can occur as sodium plays a crucial role in muscle function.
These symptoms should not be disregarded. They often manifest abruptly and can rapidly worsen. Delaying treatment could lead to life-altering or even fatal consequences. How quickly do these symptoms escalate? In some cases, severe symptoms can develop within hours, highlighting the importance of prompt recognition and action.
Taking Action: What to Do When You Suspect Severe Hyponatremia
When dealing with severe hyponatremia, time is of the essence. Here’s the recommended course of action:
- Call Emergency Services Immediately: Dial 911 (or your local emergency number) without delay. This constitutes a medical emergency. Explain the situation clearly to the dispatcher and emphasize the potential for severe hyponatremia.
- Monitor Breathing and Consciousness: Closely observe the person’s breathing and level of alertness. Report any changes to emergency personnel. If the person stops breathing, begin CPR if you are trained to do so.
- Ensure Safety and Comfort: Protect the person from injury while awaiting help. Provide comfort to the best of your ability. Clear the area of any potential hazards and try to keep the person calm.
- Provide Medical History: If you are aware of the person’s medical history, share it with the paramedics. This information will aid medical professionals in delivering optimal care. Be sure to mention any medications the person is taking or any underlying medical conditions they may have.
Why Early Diagnosis is Key
Early detection is paramount. While milder cases might respond to lifestyle adjustments and medication, severe cases necessitate immediate intervention to prevent lasting brain damage. The promptness of treatment directly impacts the likelihood of a full recovery. Speed is vital because severe hyponatremia can induce irreversible neurological damage, including brain herniation and permanent cognitive impairment. Experts believe early identification of underlying factors plays a major role in preventing severe episodes. But what specific diagnostic tests are most useful?
Understanding the Underlying Issues
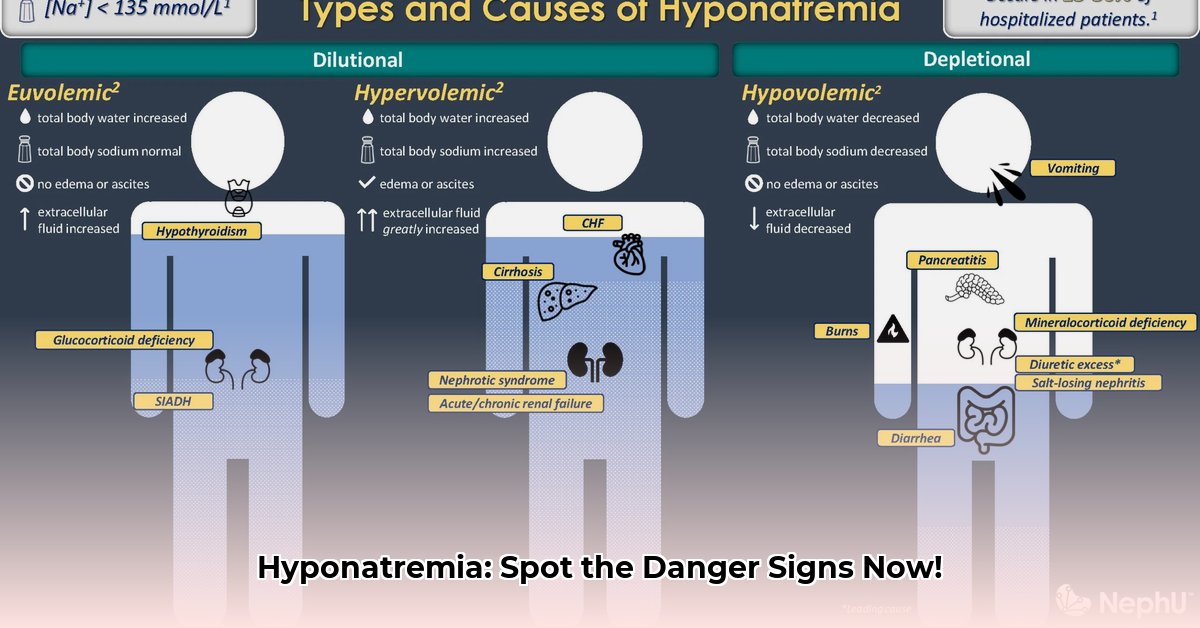
While recognizing the symptoms is crucial, comprehending why severe hyponatremia develops is equally important. The causes vary, ranging from excessive water consumption to underlying health conditions. Common causes include:
- Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH): This condition causes the body to retain water, diluting sodium levels.
- Heart Failure: The body retains fluid to compensate for decreased cardiac output, leading to hyponatremia.
- Kidney Disease: Impaired kidney function can disrupt sodium balance.
- Liver Cirrhosis: Liver disease can cause fluid retention and hyponatremia.
- Medications: Certain drugs, such as diuretics, antidepressants, and pain medications, can contribute to hyponatremia.
- Excessive Water Intake: Drinking too much water, especially during endurance events, can dilute sodium levels.
- Hormonal Imbalances: Conditions like hypothyroidism and adrenal insufficiency can affect sodium regulation.
Your doctor will employ tests to pinpoint the cause and formulate a personalized treatment plan. This plan will focus not only on stabilizing sodium levels but also on addressing the root cause of the imbalance.
The Importance of Consulting a Healthcare Professional
This information is intended as a general guide and should not substitute professional medical advice. Always seek guidance from your doctor or another qualified healthcare professional for an accurate diagnosis and to discuss treatment options. They will conduct blood tests and urine tests to ascertain the severity of your hyponatremia and devise a treatment plan tailored to your specific needs. Remember, seeking expert medical advice is vital for managing this potentially serious condition. What specific questions should you ask your doctor?
Some important questions to ask your doctor include:
- What is the underlying cause of my hyponatremia?
- What is the best treatment plan for my specific situation?
- What are the potential risks and benefits of each treatment option?
- How often will I need to have my sodium levels monitored?
- What lifestyle changes can I make to help manage my hyponatremia?
- What are the warning signs that my hyponatremia is worsening?
How to Safely Correct Hyponatremia Based on Its Subtype
Hyponatremia, characterized by low sodium levels in the blood, necessitates careful correction to avert severe complications such as osmotic demyelination syndrome (ODS). ODS is a potentially devastating neurological condition that can occur if sodium levels are corrected too quickly, leading to damage to the myelin sheath that protects nerve cells in the brain. The speed of correction is significantly influenced by the duration of low sodium levels (acute vs. chronic). More pronounced symptoms necessitate faster, yet still cautious, correction compared to asymptomatic cases. Frequent monitoring of sodium levels is essential throughout treatment. Desmopressin (DDAVP) often plays a role in safely managing sodium levels.
Understanding Hyponatremia: The Importance of Subtypes
Hyponatremia is not a uniform condition. Its treatment—how to safely correct hyponatremia based on its subtype— hinges significantly on its underlying cause and duration. Is it a sudden decrease in sodium (acute) or a gradual decline (chronic)? This distinction profoundly influences treatment strategies. Acute hyponatremia, which develops in less than 48 hours, might permit slightly faster, yet still regulated, correction, whereas chronic cases, developing over more than 48 hours, demand utmost caution. What is the typical timeline for developing chronic hyponatremia? Chronic hyponatremia develops over a period of days, weeks, or even months, allowing the brain to adapt to the low sodium levels.
Recognizing Severe Hyponatremia: When to Seek Help Immediately
Severe hyponatremia (sodium levels below 120 mmol/L, and especially below 110 mmol/L) constitutes a medical emergency. Symptoms can vary from mild nausea and confusion to
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026
- Essential Meditation Books for Beginners and Experienced Practitioners - January 27, 2026