Do you want to understand SIADH? SIADH stands for Syndrome of Inappropriate Antidiuretic Hormone Secretion. It essentially means your body retains excessive water, leading to various complications. This comprehensive guide explains SIADH and its ICD-10 code, E22.2. For more on hyponatremia ICD codes, see this helpful resource. Whether you’re a patient, caregiver, or healthcare professional, this article provides a detailed overview. We will explore causes, symptoms, diagnosis, treatment, and long-term management, empowering you to understand this nuanced condition.
Understanding SIADH: Fluid Balance and the ICD-10 Code
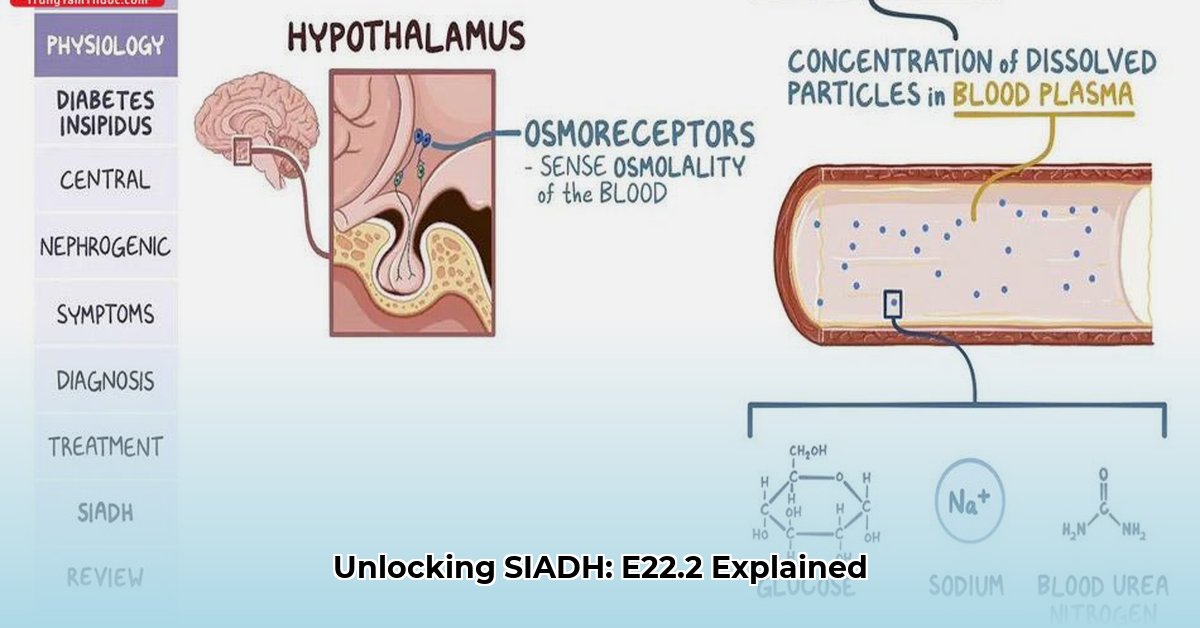
SIADH, or Syndrome of Inappropriate Antidiuretic Hormone Secretion, represents a multifaceted medical condition. While the ICD-10 code E22.2 provides a convenient label, the underlying reality is much more complex. Imagine your body’s water regulation system malfunctioning, resulting in excessive water retention and subsequent health problems—that’s SIADH in essence. It arises from the overproduction of antidiuretic hormone (ADH), also known as vasopressin. ADH is a hormone produced in the hypothalamus and released by the posterior pituitary gland that signals the kidneys to conserve water. Excessive ADH causes your body to retain too much fluid, leading to hyponatremia – dangerously low sodium levels in your blood. This electrolyte imbalance disrupts your body’s delicate homeostasis, potentially causing severe health issues.
Delving Deeper: Unraveling the Causes of SIADH
The causes of SIADH are varied and complex, often necessitating thorough investigation to identify the underlying source. Consider a plumbing system with a hidden leak; locating the origin is crucial to stopping the water damage. Common causes include:
- Tumors: Particularly small cell lung cancer (SCLC), which can inappropriately produce ADH. Other cancers such as pancreatic cancer, lymphoma, sarcoma, and prostate cancer have also been implicated.
- Central Nervous System (CNS) Disorders: Infections or injuries affecting the brain, such as meningitis, encephalitis, head trauma, stroke, or brain tumors, can disrupt ADH regulation.
- Medications: Certain drugs, including selective serotonin reuptake inhibitors (SSRIs), tricyclic antidepressants, anticonvulsants (like carbamazepine), nonsteroidal anti-inflammatory drugs (NSAIDs), and some chemotherapy agents, can trigger SIADH.
- Pulmonary Diseases: Lung diseases such as pneumonia (bacterial, viral, or tuberculosis), asthma, cystic fibrosis and respiratory failure can sometimes lead to SIADH.
- Hormonal Disorders: Conditions such as adrenal insufficiency and hypothyroidism may sometimes be associated with SIADH.
- Surgery: Postoperative pain, nausea, and stress can lead to ADH release.
- HIV/AIDS: The syndrome can occur in these patients, possibly due to opportunistic infections or medications.
Pinpointing the underlying cause is essential for effective treatment and long-term management. Current research continually explores potential triggers, expanding our understanding of this syndrome. While genetic factors are suspected to play a role in specific cases, further research is needed to fully elucidate their impact. Other less common causes include Guillain-Barré syndrome, acute intermittent porphyria, and ectopic ADH production by non-cancerous tissues. Neurological conditions such as multiple sclerosis can also sometimes lead to SIADH.
Recognizing the Warning Signs: Symptoms of SIADH
The symptoms of SIADH exhibit considerable variability based on the severity of hyponatremia (low sodium levels). In mild cases, symptoms may be subtle or even absent, consisting of headaches, muscle cramps, or persistent nausea. More severe cases can manifest dramatically, presenting with:
- Neurological Symptoms: Confusion, lethargy, disorientation, irritability, hallucinations, seizures, coma.
- Gastrointestinal Symptoms: Nausea, vomiting, loss of appetite.
- Musculoskeletal Symptoms: Muscle weakness, cramps, tremors.
- Fluid Overload Symptoms: Edema (swelling), weight gain.
These severe symptoms result from the disruption of electrolyte balance affecting brain function. The speed at which hyponatremia develops also impacts the severity of symptoms, where rapid declines in sodium levels tend to be more symptomatic. If you experience these symptoms, particularly if they seem unexplained, seeking immediate medical attention is crucial. Early detection and treatment are key to preventing serious complications. Severe hyponatremia can lead to brain swelling (cerebral edema), which can be life-threatening.
Diagnosing SIADH: A Multi-Faceted Approach
Diagnosing SIADH entails a combination of clinical evaluation and laboratory tests. Doctors typically begin with a thorough physical examination and medical history assessment, followed by specific diagnostic tests:
- Blood Tests: Focus on serum sodium levels, serum osmolality (concentration of particles in the blood), and ADH levels. Low serum sodium and low serum osmolality, combined with inappropriately elevated ADH levels, are indicative of SIADH.
- Urine Tests: Urine osmolality and urine sodium levels help assess the kidney’s ability to concentrate urine and excrete sodium. High urine osmolality and urine sodium in the setting of low serum osmolality further support the diagnosis.
- Exclusion of Other Conditions: It’s crucial to rule out other conditions that can cause hyponatremia, such as adrenal insufficiency, hypothyroidism, kidney disease, and heart failure.
- Imaging Studies: Chest X-rays or CT scans may be necessary to identify underlying conditions like lung tumors or pulmonary infections. MRI scans of the brain may be used to rule out CNS disorders.
- Fluid Status Assessment: Evaluating the patient’s fluid status to determine if they are euvolemic (normal fluid volume), hypovolemic (dehydrated), or hypervolemic (fluid overloaded) is also important. SIADH is typically associated with euvolemia or mild hypervolemia.
These investigations not only assist in diagnosing SIADH but also help determine the underlying cause—a crucial step in creating an effective treatment plan. The diagnostic process sometimes requires a process of elimination, where doctors rule out other conditions with similar symptoms before confirming a diagnosis of SIADH. Water loading tests, where a patient is given a specific amount of water and then monitored for their ability to excrete it, can be used to further confirm the diagnosis in complicated cases.
Managing SIADH: Restoring Electrolyte Balance
Treatment for SIADH is tailored to the underlying cause and the severity of hyponatremia. The primary goals are to correct the sodium imbalance and address the underlying cause where possible. Here are common treatment strategies:
- Fluid Restriction: Often the first-line treatment. Limiting daily fluid intake (typically to 800-1000 ml per day) helps reduce water retention and gradually increase serum sodium levels.
- Sodium Supplementation: In some cases, increasing sodium intake through diet or salt tablets may be recommended.
- Hypertonic Saline: For severe hyponatremia with neurological symptoms, intravenous administration of hypertonic saline (3% NaCl) may be necessary to rapidly increase serum sodium levels. This must be done cautiously to avoid overly rapid correction, which can lead to a neurological condition called osmotic demyelination syndrome (ODS).
- Medications:
- Loop Diuretics: Such as furosemide, can help promote water excretion by the kidneys. However, they must be used carefully in conjunction with sodium supplementation to avoid further sodium loss.
- Vaptans: These medications (e.g., tolvaptan, conivaptan) are ADH receptor antagonists that block the action of ADH on the kidneys, promoting water excretion without sodium loss. They are typically reserved for more severe or refractory cases of SIADH.
- Treating the Underlying Cause: Addressing the underlying cause of SIADH is crucial for long-term management. This may involve surgery, chemotherapy, or radiation therapy for tumors; antibiotics for infections; or discontinuing offending medications.
The treatment approach is tailored to each individual case, considering the person’s overall health, the severity of their symptoms, and the underlying cause of SIADH. Regular monitoring of serum sodium levels is essential to guide treatment and prevent complications. It is important that correction of hyponatremia is gradual to avoid neurological sequelae.
The ICD-10 Code E22.2: A Clinical Tool
The ICD-10 code E22.2 serves as a standardized way to classify SIADH for billing, statistical, and record-keeping purposes. However, it’s important to recognize that this code provides only a snapshot of the condition. Given that SIADH is often secondary to various underlying causes, additional ICD-10 codes are typically added to provide a more comprehensive clinical picture and assist in appropriate and accurate billing. For example:
- If SIADH is caused by small cell lung cancer: Codes for both SIADH (E22.2) and small cell lung cancer (C34.x) would be used.
- If SIADH is drug-induced: Codes for both SIADH (E22.2) and the specific drug involved (T codes for poisoning by drugs) would be used.
This more detailed coding approach ensures accurate documentation and helps healthcare providers tailor treatment plans to the individual’s specific circumstances. A comprehensive approach is crucial for effective treatment, informative research, and accurate public health statistics.
Living Well with SIADH: Long-Term Management
The long-term outlook for individuals with SIADH depends heavily on the underlying cause and the effectiveness of its management. If the underlying condition, such as a tumor, can
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026