Are you grappling with a recent hyponatremia diagnosis? Feeling overwhelmed? You’re not alone. Low sodium in the blood, or hyponatremia, is a common condition, and this guide is designed to equip you with the knowledge and tools to understand and manage it effectively. We’ll break down the complexities of hyponatremia into easy-to-understand terms, covering its causes, symptoms, treatment options, and prevention strategies. Beyond simply defining the condition, our goal is to empower you to actively participate in your healthcare and confidently navigate the path to recovery. We’ll outline essential lifestyle adjustments, explain what to expect during doctor visits, and provide actionable steps you can take to regain control of your health and prevent future occurrences. For more information, see this helpful patient handout.
Understanding Hyponatremia: More Than Just Low Sodium
Let’s delve into the fundamentals of hyponatremia. In essence, it signifies that the sodium levels in your blood are lower than normal. Sodium, a vital electrolyte, plays a crucial role in maintaining fluid balance, regulating nerve and muscle function, and controlling blood pressure. Think of sodium as a conductor, orchestrating various bodily functions; when its levels are disrupted, various systems can be thrown off balance.
Consider your body as a carefully calibrated system constantly regulating fluids. Sodium is a critical element in this balancing act. When this equilibrium is disturbed, hyponatremia can develop. It’s important to recognize that hyponatremia is not a disease in itself, but rather an indicator of an underlying issue affecting fluid and sodium regulation. Grasping this concept is the first step towards effective management and improved well-being. What are the potential complications of prolonged, untreated hyponatremia?
Identifying the Root Causes: A Matter of Fluid and Sodium Balance
Several factors can contribute to a drop in sodium levels. Envision a seesaw: if there’s an excess of fluid or a deficiency of sodium, the equilibrium is disrupted. Hyponatremia is generally categorized into three primary types:
-
Hypovolemic Hyponatremia: This occurs when both fluid and sodium are lost from the body, often due to conditions like vomiting, diarrhea, excessive sweating, or diuretic use. Imagine a leaky bucket – the body is losing essential fluids and electrolytes, leading to an imbalance.
-
Hypervolemic Hyponatremia: In this case, the seesaw is tipped towards fluid overload. The body retains too much fluid, diluting the sodium concentration. This is often associated with conditions such as heart failure, kidney disease, or liver cirrhosis, where the body’s ability to regulate fluid balance is impaired.
-
Euvolemic Hyponatremia: This type presents a unique challenge, as the overall fluid levels in the body are seemingly normal. However, the sodium is diluted due to various factors, including syndrome of inappropriate antidiuretic hormone secretion (SIADH), certain medications, or hormonal imbalances. Think of it as adding too much water to a saltwater solution, even though the total volume appears normal.
It’s crucial to understand that pinpointing the precise cause of hyponatremia can be complex. Doctors often employ a combination of tests, medical history review, and physical examination to identify the underlying factor and determine the appropriate course of treatment.
Recognizing the Warning Signs: When to Seek Prompt Medical Evaluation
The symptoms of hyponatremia can vary widely, ranging from mild and subtle to severe and life-threatening, depending on the degree of sodium depletion. Paying close attention to your body and seeking medical attention when necessary is paramount.
Mild Symptoms: These initial indicators can be easily overlooked and may include fatigue, headache, nausea, loss of appetite, muscle cramps, or mild cognitive impairment. While not immediately alarming, it’s advisable to inform your doctor about these symptoms. They may recommend simple lifestyle adjustments or suggest further monitoring.
Moderate Symptoms: As sodium levels decline further, more pronounced symptoms may emerge, such as vomiting, muscle weakness, confusion, lethargy, or gait disturbances. These signs warrant prompt medical evaluation. Delaying treatment can lead to more serious complications.
Severe Symptoms: In severe cases, hyponatremia can trigger seizures, altered mental status, coma, or even death. These are medical emergencies that require immediate intervention. If you experience any of these symptoms, call emergency services immediately.
Here’s a concise summary of symptoms and recommended actions:
| Symptom Severity | Symptoms | When to Seek Help |
|---|---|---|
| Mild | Headache, fatigue, nausea, loss of appetite, muscle cramps, mild confusion | Inform your doctor, monitor symptoms, and follow their recommendations |
| Moderate | Vomiting, muscle weakness, confusion, lethargy, gait disturbances | Seek medical attention promptly |
| Severe | Seizures, altered mental status, coma | Call emergency services immediately (911 or your local emergency number) |
Diagnostic Procedures: Confirming Hyponatremia and Identifying the Cause
Diagnosing hyponatremia typically involves a simple blood test to measure your serum sodium levels. This test provides a clear indication of whether your sodium levels are within the normal range. In addition to the blood test, your doctor may order further investigations to determine the underlying cause of the hyponatremia. These tests may include urine tests, kidney function tests, hormone level assessments, and imaging studies. What are the primary risk factors for developing hyponatremia?
Treatment Strategies: Restoring Sodium Balance Safely
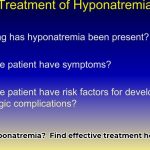
The primary goal of hyponatremia treatment is to gradually and safely restore sodium levels to the normal range. Rapid correction of hyponatremia can be dangerous and may lead to serious neurological complications. Treatment plans are tailored to the individual, depending on the severity of the hyponatremia, the underlying cause, and the patient’s overall health status. Your doctor may recommend a combination of the following approaches:
-
Fluid Restriction: Limiting fluid intake can help to increase sodium concentration in the blood, particularly in cases of hypervolemic hyponatremia.
-
Sodium Supplementation: In some cases, sodium can be administered orally or intravenously to replenish depleted levels.
-
Medication Adjustments: If certain medications are contributing to hyponatremia, your doctor may adjust the dosage or switch to alternative medications.
-
Treatment of Underlying Conditions: Addressing the underlying cause of hyponatremia, such as heart failure or kidney disease, is crucial for long-term management.
Long-Term Management: Sustainable Lifestyle Adjustments
Adopting long-term lifestyle modifications can play a significant role in managing hyponatremia, preventing future episodes, and improving overall well-being. These adjustments may include:
-
Dietary Modifications: Consulting with a registered dietitian can help you optimize your sodium intake. This doesn’t necessarily mean eliminating sodium entirely, but rather finding a healthy balance. Focus on consuming a balanced diet with adequate sodium from natural sources, while limiting processed foods high in sodium.
-
Medication Management: Adhere to your doctor’s instructions regarding all medications, as some can affect sodium levels. Be sure to inform your doctor about all medications you are taking, including over-the-counter drugs and supplements.
-
Hydration Management: Maintain a healthy fluid intake. Avoid extremes – both dehydration and overhydration can disrupt electrolyte balance.
-
Alcohol Consumption: Moderate alcohol consumption is recommended, as excessive alcohol intake can impair fluid balance and sodium regulation.
The Importance of Ongoing Monitoring and Follow-Up Care
Regular blood tests are essential to monitor your sodium levels and assess the effectiveness of treatment. Close collaboration with your healthcare provider is crucial for long-term management. They will guide you through the process, monitor your progress, and address any concerns or questions you may have. What are the advantages of consistent medical supervision?
Addressing Common Questions and Concerns
-
Q: Is hyponatremia preventable? A: In many cases, yes. Maintaining a healthy lifestyle, including a balanced diet, appropriate hydration, and careful medication management, can reduce your risk of developing hyponatremia.
-
Q: What are the potential long-term health risks associated with hyponatremia? A: If left untreated or poorly managed, hyponatremia can lead to serious complications, including neurological damage, seizures, coma, and even death.
-
Q: How long does it take to recover from hyponatremia? A: Recovery time varies depending on the underlying cause, the severity of the condition, and the individual’s overall health. Your doctor can provide a more accurate estimate based on your specific circumstances.
Remember, understanding hyponatremia is the first step towards effective management and improved health. Your healthcare team is your partner in this journey. By actively participating in your care, asking questions, and adhering to your treatment plan, you can significantly improve your well-being and quality of life. How can open communication with your doctor enhance treatment outcomes?
Preventing Hyponatremia from Diuretic Use: A Comprehensive Patient Guide
Key Takeaways:
- Hyponatremia is a potential side effect of diuretic use, but with careful monitoring and proactive measures, it can be prevented.
- Awareness of risk factors, recognition of early symptoms, and adherence to medical advice are crucial for preventing severe hyponatremia.
- Regular blood tests, open communication with your doctor, and appropriate lifestyle adjustments are essential for effective management.
- Understanding how to prevent hyponatremia from diuretic use empowers you to actively participate in your healthcare and minimize potential risks.
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026