Yes, you can generally take Tylenol (acetaminophen) before a colonoscopy, but it’s crucial to consult your doctor for specific instructions. Your doctor can assess your individual health situation and provide tailored guidance.
Key Considerations Before Your Colonoscopy
- Dosage and Timing: Follow your doctor’s recommended dosage and timing for any medication.
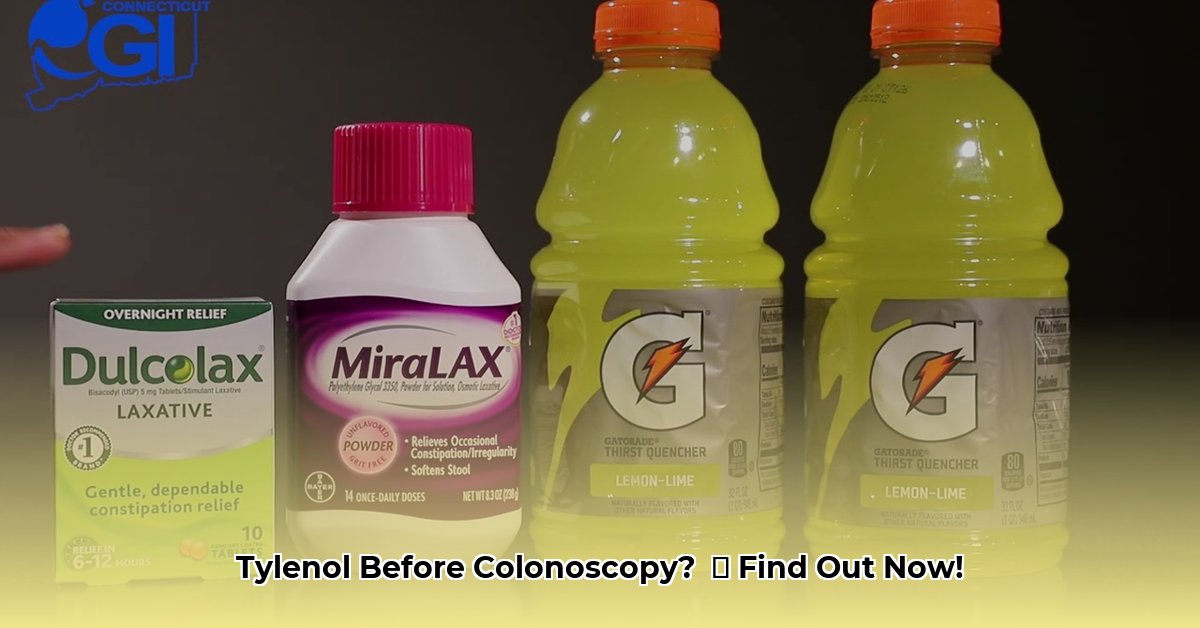
- Medications to Avoid: Avoid blood thinners (e.g., Plavix, Effient, Eliquis, Xarelto, Coumadin/Warfarin, aspirin), NSAIDs (ibuprofen, naproxen), iron supplements, fish oil, certain opioid medications, anti-diarrheal medications, diuretics, and some herbal remedies unless specifically cleared by your physician.
- Colonoscopy Prep: Do not substitute Tylenol for your prescribed colonoscopy preparation.
- Post-Colonoscopy Discomfort: Expect some bloating, cramping, and gas after the procedure. This is normal and usually temporary.
Why Your Doctor’s Advice is Essential
While this guide provides helpful information, it’s not a substitute for personalized medical advice. Your doctor considers several factors when advising you about medications before a colonoscopy:
- Other Medications: Potential interactions between Tylenol and your other medications (prescription or over-the-counter) could cause complications.
- Existing Health Conditions: Conditions like liver problems might require adjustments to medication usage. Even Tylenol can be harmful if you exceed the recommended daily dose (4,000 mg).
- Specific Colonoscopy Prep: Some preps may interact with Tylenol, potentially decreasing their effectiveness, so following your doctor’s instructions is important.
- Individual Health Profile: Your unique health history plays a vital role in the advice your doctor provides.
Understanding Medication Restrictions
Certain medications are restricted before a colonoscopy because they can interfere with the procedure or increase the risk of complications. For example:
- Blood Thinners: These medications (e.g., Plavix, Effient, Eliquis, Xarelto, Coumadin/Warfarin, aspirin) can increase the risk of bleeding during the procedure.
- NSAIDs (e.g., ibuprofen, naproxen): Similar to blood thinners, NSAIDs can also elevate bleeding risk.
- Iron Supplements and Fish Oil: These can obscure the colon lining, making it difficult for the doctor to get a clear view during the procedure.
- Certain Opioids, Anti-diarrheals, and Diuretics: These can impact bowel function, interfere with the bowel prep, or affect electrolyte balance, respectively.
- Herbal Remedies/Supplements: Some herbal supplements can interact with anesthesia or the bowel prep, leading to unforeseen issues.
Your doctor will likely advise you to stop taking these medications several days or a week before your procedure. The exact timeframe depends on you and the specific medication.
Sedation and Pain Relief During the Colonoscopy
Most colonoscopies use moderate sedation, a combination of a sedative and a painkiller to manage any potential discomfort. You’ll likely feel relaxed and drowsy and probably won’t remember the procedure. While rare, a propofol injection (often used for sedation) can cause a brief stinging sensation. However, a local anesthetic can numb the area beforehand. Other sedation options, like deep sedation or general anesthesia, are available if needed and will be discussed with you.
Managing Post-Colonoscopy Discomfort
After the procedure, you might experience some bloating, cramping, and gas. This is a normal reaction as your digestive system recovers. Walking around can often help alleviate these symptoms. While Tylenol can be used for minor discomfort post-procedure, always consult your doctor about the appropriate dosage and timing.
Medications and Your Colonoscopy: A Quick Reference
| Medication Category | Generally Permitted? | Notes |
|---|---|---|
| Acetaminophen (Tylenol) | Usually | Always check with your doctor about the appropriate dosage and timing. |
| NSAIDs (Ibuprofen, Naproxen, Aspirin) | Usually not | Avoid for several days before the procedure due to potential bleeding risk. Consult your doctor. |
| Blood Thinners | Consult Your Doctor | Requires discussion with your physician well in advance. |
| Iron Supplements | Usually not | May need to discontinue temporarily. Check with your doctor. |
| Fish Oil | Consult Your Doctor | Discuss with your physician due to potential blood-thinning effects. |
| Herbal Remedies/Supplements | Consult Your Doctor | Some may interfere; discuss all supplements with your physician. |
| Anti-diarrheal Medications | Usually not | Can interfere with the bowel prep; consult your doctor. |
| Opioids (Pain Medications) | Consult Your Doctor | Discuss potential impacts on bowel prep and bleeding risk with your doctor. |
| Diuretics | Consult Your Doctor | Discuss potential effects on electrolyte balance with your doctor. |
Staying Informed
Medical understanding is constantly evolving. Ongoing research suggests that certain pain relievers may have subtle effects on the colonoscopy process. While current guidelines generally indicate Tylenol’s safety, it’s important to stay updated and consult your doctor about new information.
Disclaimer: This information is for educational purposes only and not a substitute for professional medical advice. Always consult with your doctor or other qualified health professional for any health concerns or before making any decisions related to your health or treatment.
- The TM Book Offers an Essential Guide to Meditation. - March 4, 2026
- Transcendental Meditation Books Guiding Your Journey to Deeper Practice - March 3, 2026
- Your TM Meditation Book Explores Its Benefits and History - March 2, 2026