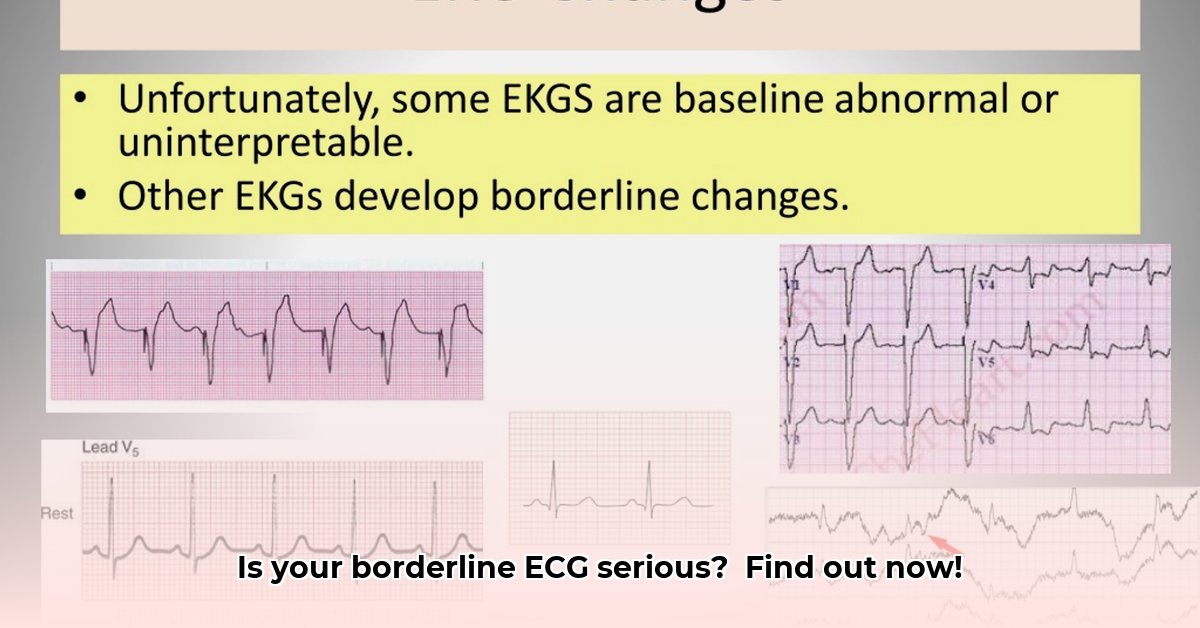
Got a borderline ECG result and feeling a little freaked out? Don’t worry, you’re not alone. A lot of people get nervous when they see something like that on a medical report. This article will help you understand what a borderline ECG means, what’s considered normal, and what you should do next. We’ll explain things in plain English, so you don’t need a medical degree to get it. We’ll also talk about how to lower your risk for heart problems and give you the information you need to take care of your heart. Let’s break this down together and get you feeling more confident about your heart health.
Is Borderline ECG Serious? Understanding the Implications
So, you got a “borderline” result on your ECG. What now? Panic? Not necessarily. Let’s clear up some things. A borderline ECG isn’t a diagnosis; it’s more like a doctor saying, “Let’s investigate further.” It means your heart’s electrical activity showed some minor variations. These are subtle changes, not major alarms. It doesn’t automatically mean you have a serious heart problem, but you should have it checked out. Minor irregularities in heart rhythm can be caused by something as simple as stress or side effects from a medication.
Decoding Your ECG: What Do Borderline Findings Really Mean?
Think of your heart’s electrical system as a precisely timed orchestra. An electrocardiogram (ECG or EKG) records this performance. A normal ECG shows a smooth, consistent rhythm. A borderline ECG suggests a few musicians might be slightly off-key. There might be slight pauses, or a few instruments not quite in sync. These minor irregularities don’t always mean something’s seriously wrong, but they warrant a closer look.
A borderline ECG isn’t a definitive answer; it’s a question mark. It’s a signal that more information is needed. Many innocent reasons can cause it – stress, a medication, or a temporary imbalance in your body’s electrolytes (minerals like potassium). It’s not a simple yes or no answer. It needs a more thorough examination.
Common Culprits: What Might Cause a Borderline ECG?
Many things can cause a slightly off ECG reading. Think of it like a car needing a tune-up; some minor adjustments might be all that’s needed. Here are a few possibilities:
- Electrolyte Imbalances: Your body’s chemistry plays a big role in heart rhythm. Changes in levels of potassium, sodium, calcium or magnesium can slightly alter your ECG. These electrolytes are the “fuel” for your heart’s electrical system. If the fuel mix is off, the engine might not run perfectly smoothly.
- Medications: Certain medications, including some over-the-counter drugs and supplements, can affect your heart’s rhythm as a side effect. This is fairly common and often easily addressed.
- Stress and Anxiety: Stress and anxiety can show up on an ECG. The body reacts to stress in many ways, and sometimes this shows as minor heart rhythm changes.
- Technical Factors: Human error or equipment issues can happen. If the ECG electrodes weren’t perfectly placed on your chest, or if there was electrical interference, it could lead to a slightly inaccurate reading.
- Underlying Heart Conditions: While less likely with a borderline result, there’s always the possibility of an underlying heart condition. This is why further investigation is so important. Studies show that a significant percentage of ECGs show borderline results, highlighting the need for careful evaluation.
Proactive Steps: What to Do If Your ECG Comes Back Borderline
Don’t panic! The most important thing is to talk to your doctor. Don’t try to diagnose yourself based on a single test result. Your physician will consider your whole health picture – your ECG results, any symptoms you’re experiencing, your medical history, and your lifestyle.
Further Investigations: Getting a Clearer Picture of Your Heart Health
Depending on your situation, your doctor may recommend additional tests. These aren’t necessarily signs that anything is seriously wrong; they are simply further steps to ensure your heart’s in good shape. These might include:
- A Repeat ECG: Sometimes, a simple second ECG will show the first result was just a slight anomaly.
- A Stress Test: This involves exercising while having your heart monitored. It shows how your heart handles physical activity and can reveal problems that don’t appear at rest.
- An Echocardiogram: This is an ultrasound of your heart. It creates images of your heart’s structure and function, helping to check for any abnormalities in the valves or chambers.
- A Holter Monitor: This is a portable ECG you wear for 24-48 hours (or even longer in some cases). It continuously records your heart’s activity, giving doctors a more comprehensive view of your heart rhythm than a single snapshot.
- Event Recorder: Similar to a Holter monitor, but worn for a longer period (weeks or even months). You activate it when you feel symptoms.
- Blood Tests: These can help rule out other potential causes, such as thyroid problems or electrolyte imbalances.
The goal here isn’t to worry you but to be proactive about your heart health. Preventative care is key!
Assessing Your Risk: Understanding the Bigger Picture
So, back to the original question: Is a borderline ECG serious? The most accurate answer is: it depends. The risk level depends on several factors: your overall health, whether or not you’re having any symptoms, and your family history of heart issues.
Here’s a simplified look at the potential risk:
| Factor | Risk Level | Considerations |
|---|---|---|
| Borderline ECG + Symptoms | Medium to High | Requires prompt evaluation to determine cause of symptoms and borderline ECG. |
| Borderline ECG + No Symptoms | Low to Medium | May require further monitoring and investigation based on individual risk factors. |
Remember, a borderline ECG result is never a definitive diagnosis. It simply calls for more information. Don’t hesitate to reach out to your doctor with any questions or concerns. Your proactive approach to your heart health is vital. Seeking professional advice will provide peace of mind and help you stay healthy.
Interpreting Borderline ECG Results: A Step-by-Step Guide
Key Takeaways:
- A borderline ECG isn’t a diagnosis, but a reason to investigate further. It suggests subtle irregularities in your heart rhythm.
- Many factors can lead to borderline ECGs, including stress, caffeine, medications, and even minor technical issues during testing.
- Your doctor will need your complete medical history and a thorough physical exam to properly interpret your ECG results.
- Further tests might be recommended, such as a repeat ECG, a Holter monitor for extended rhythm tracking, or other cardiac assessments.
- Knowing your risk factors is essential for determining the appropriate level of concern. Early lifestyle adjustments can significantly improve heart health outcomes.
What Does a Borderline ECG Actually Mean? Understanding the Implications
Think of your ECG as a snapshot of your heart’s electrical activity. A borderline result means the picture isn’t perfectly clear. It shows some minor deviations from the typical pattern, but they aren’t significant enough to make a definitive diagnosis outright. It’s like seeing a faint smudge on a photograph – you need a closer look to know if it’s important.
So, is it serious? Not necessarily. Many things can cause a borderline ECG, from temporary issues like stress or dehydration to medication side effects. Sometimes, it’s a simple technicality during the recording. However, ignoring it isn’t wise. Consulting your doctor for a proper evaluation is key.
How to Interpret Borderline ECG Results and Determine Next Steps: A Practical Guide
- Discuss your results with your doctor: This is the most important step. Your doctor will consider your ECG in conjunction with your personal health history, symptoms (if any), and any risk factors you might have (family history of heart disease, high blood pressure, diabetes, smoking).
- Identify potential causes: Your doctor will work to rule out temporary or easily corrected causes, such as stress, lack of sleep, recent strenuous activity, dehydration, or certain medications and supplements.
-
Consider additional testing: Depending on your individual circumstances, additional tests may be recommended. These could include:
- A repeat ECG: A simple retake can sometimes resolve ambiguities.
- Holter monitoring: Wearing a portable ECG monitor for 24 to 48 hours to capture longer periods of heart activity.
- Event Recorder: A monitor worn for several weeks that you activate when you experience symptoms.
- Echocardiogram: An ultrasound of the heart to assess its structure and function.
- Stress test: Measures heart function during physical exertion to reveal any underlying problems.
- Cardiac CT scan: Provides detailed images of the heart and blood vessels.
- Blood tests: To check for electrolyte imbalances, thyroid issues, and other factors.
-
Lifestyle adjustments: Your doctor might suggest lifestyle modifications such as managing stress, incorporating regular exercise, maintaining a healthy diet, limiting caffeine and alcohol consumption, and quitting smoking. These changes can sometimes improve heart health and rhythm.
- Ongoing monitoring: In some cases, regular follow-up ECGs or other cardiac tests may be necessary to monitor your heart
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026
- Essential Meditation Books for Beginners and Experienced Practitioners - January 27, 2026