Got a “borderline” ECG result? Don’t panic! It indicates your heart’s rhythm showed something slightly unusual, but it’s not necessarily cause for alarm. This isn’t a diagnosis itself, more like a “let’s take a closer look” sign from your doctor. This article will explain what a borderline ECG means, common causes, and, most importantly, what you should do next. You’ll learn when you need to seek immediate medical attention, how to effectively communicate with your doctor about the results, and actionable steps you can take to promote and maintain optimal heart health. Many times, a borderline ECG is harmless, but understanding it empowers you to take control of your heart health journey.
Decoding a Borderline ECG: Symptoms, Causes, and Comprehensive Next Steps
A borderline ECG result can understandably cause anxiety, but it’s crucial to remember that it doesn’t automatically signify a serious underlying condition. Let’s delve into what a borderline ECG truly means and provide you with a clear roadmap of what steps you should take.
Demystifying the Borderline ECG: Understanding the Fundamentals
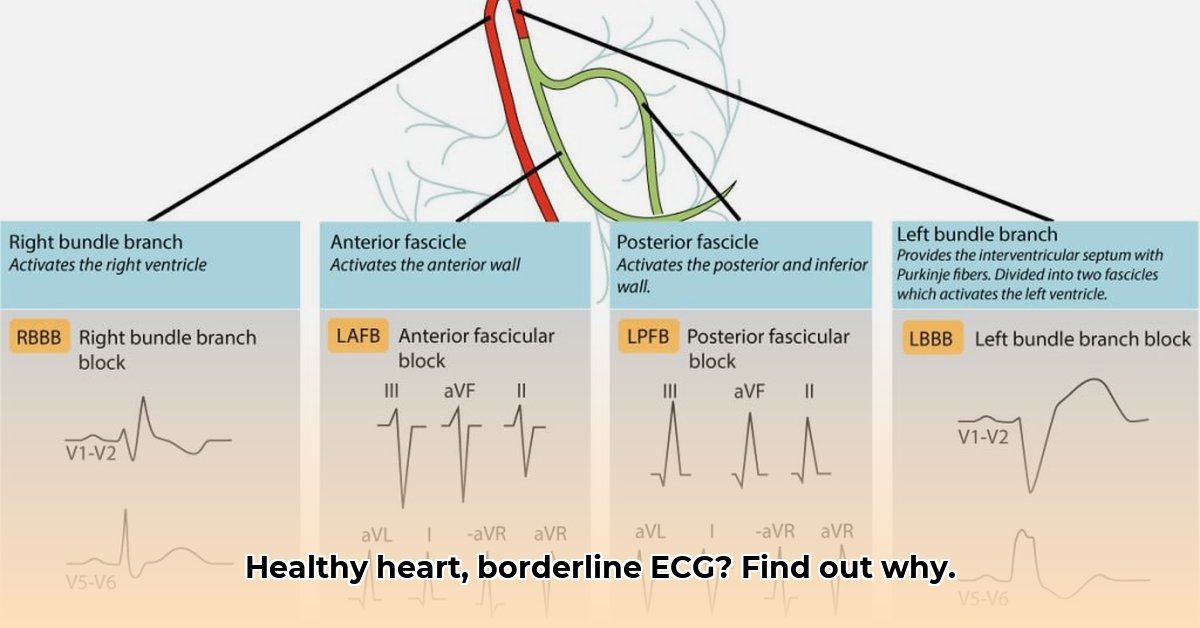
Envision your heart’s electrical system as a highly intricate and finely tuned orchestra. An electrocardiogram (ECG) serves as a recording of this orchestra’s performance, capturing the complex interplay of electrical signals that govern each heartbeat. A “borderline” ECG simply indicates that the recording reveals some slightly atypical notes or variations in the rhythm, but not to a degree that definitively confirms a problem or guarantees that everything is perfectly normal. It’s akin to a conductor noticing a few musicians playing slightly off-beat – it’s not a full-blown crisis demanding immediate intervention, but it does warrant a more in-depth assessment. It’s inconclusive – additional data and context are required before a definitive determination can be made. Consider it a “maybe” rather than a conclusive “yes” or “no.” This nuanced interpretation suggests the possibility of subtle deviations from the norm, but doesn’t necessarily indicate a serious heart problem. In fact, many seemingly healthy individuals exhibit borderline ECGs at some point in their lives.
Unveiling Potential Causes of Borderline ECG Readings
There exists a wide array of potential reasons why your ECG might register a borderline result, and the majority of these causes are entirely benign and pose no threat to your health. To illustrate this point, consider the fact that your heart’s rhythm is remarkably sensitive and susceptible to even subtle influences. Everyday stressors, such as work deadlines or personal challenges, can temporarily alter your heart rhythm, manifesting as a borderline result on your ECG. Likewise, minor imbalances in your body’s electrolytes (such as potassium, sodium, calcium, and magnesium), which play critical roles in maintaining proper heart function, can subtly impact your heart’s electrical patterns. Even certain medications, including over-the-counter remedies and supplements, can elicit similar effects. It is important to note that, while less frequent, a borderline ECG may occasionally serve as an early indicator of an underlying heart condition or other health issue. For example, it could be related to high blood pressure, an overactive thyroid, or even sleep apnea. If you experience concomitant symptoms such as chest pain, severe shortness of breath, dizziness, or fainting, it’s imperative that you seek immediate medical attention. These symptoms necessitate prompt evaluation to rule out any potentially life-threatening conditions.
This is precisely why further investigation is so crucial – to definitively rule out any serious underlying issues and provide you with peace of mind.
Decoding Results: The ECG is Not a Stand-Alone Diagnostic Tool
It’s essential to understand that a borderline ECG is not a diagnosis in and of itself. Rather, it serves as a signal that further investigation may be warranted to gain a more comprehensive understanding of your heart health. Your doctor will not base a diagnosis solely on the ECG results; instead, they will meticulously consider the complete clinical picture, taking into account your symptoms, your medical history (including any family history of heart conditions), and your lifestyle factors. The ECG is merely one piece of the intricate puzzle that your physician must assemble to arrive at an accurate assessment of your health. Your physician needs to interpret the results within the context of your complete medical history and any symptoms you are currently experiencing. This process is referred to as “clinical correlation,” and it is absolutely essential for ensuring a proper and well-informed interpretation.
How to Interpret Borderline ECG Results and Next Steps: Your Comprehensive Action Plan
Your subsequent steps will be tailored to your specific situation and guided by your doctor’s expert advice. However, here’s a comprehensive guideline outlining the general course of action you can expect: Your doctor may recommend additional diagnostic tests to gather more information and gain a clearer picture of your heart’s function. These tests might include a stress test (to evaluate how your heart performs under physical exertion), an echocardiogram (an ultrasound imaging technique used to visualize the structure and function of your heart), or a Holter monitor (a small, portable device used to continuously monitor your heart rhythm over a period of 24 to 48 hours).
- Schedule a Consultation with Your Doctor: If you’ve received a borderline ECG result, the most crucial step is to schedule a follow-up appointment with your doctor to discuss the findings in detail. This consultation is essential for obtaining personalized guidance and having any questions or concerns you may have thoroughly addressed. Don’t hesitate to ask for clarification on anything you don’t fully understand.
- Be Vigilant for Warning Signs: In addition to scheduling a follow-up appointment, it’s imperative that you remain vigilant and attentive to any potential warning signs or concerning symptoms. If you experience any of the following symptoms, seek immediate medical attention without delay:
- Chest pain or discomfort (angina)
- Shortness of breath (dyspnea)
- Dizziness or lightheadedness
- Fainting or loss of consciousness (syncope)
- A racing, fluttering, or irregular heartbeat (palpitations)
- Undergo Further Testing (If Recommended): Depending on your doctor’s comprehensive assessment of your individual situation, they may recommend that you undergo further diagnostic testing to evaluate your heart health more thoroughly. These tests may include:
- Stress Test: This test measures your heart’s response to physical exercise or pharmacological stress, providing valuable information about its function and blood flow.
- Echocardiogram: This non-invasive imaging technique utilizes ultrasound waves to create detailed images of your heart’s structure and function, allowing your doctor to assess the size, shape, and movement of your heart chambers and valves.
- Holter Monitor: This small, portable device is worn continuously for 24 to 48 hours, recording your heart’s electrical activity and rhythm over an extended period. This allows your doctor to identify any intermittent or infrequent arrhythmias that may not be detected during a standard ECG.
- Event Recorder: Similar to a Holter monitor, an event recorder is worn for a longer period (typically 30 days) and is activated only when you experience symptoms. This allows you to capture and record any unusual heart activity that occurs sporadically.
- Implement Lifestyle Adjustments (If Necessary): Based on the overall assessment of your health status, your doctor may recommend certain lifestyle modifications to promote and maintain optimal heart health. These adjustments may include:
- Stress management techniques (such as yoga, meditation, deep breathing exercises, or counseling)
- Regular physical activity (aim for at least 30 minutes of moderate-intensity exercise most days of the week)
- A heart-healthy diet (emphasizing fruits, vegetables, whole grains, lean protein, and healthy fats)
- Weight management (if needed, work towards achieving and maintaining a healthy weight)
- Smoking cessation (if applicable, seek support and resources to quit smoking)
- Limiting alcohol consumption (if you choose to drink, do so in moderation)
Addressing Concerns: Understanding the Implications of Your Results
It’s perfectly natural and understandable to experience feelings of anxiety, worry, or uncertainty after receiving a borderline ECG result. However, it’s important to remember that many individuals have borderline ECG results without having any underlying heart problems or significant health issues. In fact, borderline ECGs are more common than you might initially think. A proactive and thorough follow-up with your doctor will help to address any concerns you may have, alleviate your anxiety, and ensure the early detection and management of any potential underlying issues.
Several factors can influence the likelihood that a borderline ECG may reflect an underlying cardiac condition. It’s important to bear in mind that this is not an exhaustive list, and your doctor will consider all aspects of your health and lifestyle when assessing your individual risk.
| Factor | Possible Impact on Risk |
|---|---|
| Strong Family History of Heart Disease | Increased Risk |
| Pre-existing Health Conditions (e.g., high blood pressure, diabetes, high cholesterol) | Increased Risk |
| Significant or persistent Symptoms (chest pain, shortness of breath, palpitations, dizziness) | Increased Risk |
| High Stress Levels/Unhealthy Lifestyle (e.g., poor diet, lack of exercise, smoking) | Potentially Increased Risk |
| Electrolyte Imbalances (e.g., low potassium, high calcium) | Potentially Increased Risk |
| Certain Medications (e.g., diuretics, antidepressants, antiarrhythmics) | Potentially Increased Risk |
| Structural Heart Abnormalities | Increased Risk |
| History of |
- Top Rated Meditation Books to Deepen Your Practice - February 5, 2026
- Good Mindfulness Books For A Calmer, Happier Everyday Life - February 4, 2026
- Recommended Meditation Books for Beginners and Experienced Practitioners - February 3, 2026