Hyponatremia, characterized by abnormally low sodium levels in the blood, poses a significant clinical challenge in individuals with cirrhosis, a chronic liver disease. Effective management hinges on a thorough understanding of its complex causes, accurate and timely diagnosis, personalized treatment strategies, and precise ICD-10 coding. For more information on ICD-10 codes related to hyponatremia, see this helpful resource: ICD-10 codes. This comprehensive guide provides an in-depth overview of hyponatremia in the context of cirrhosis, encompassing its pathophysiology, classification, diagnostic workup, therapeutic options, prognostic implications, and the role of ICD-10 codes, particularly E87.1. This guide emphasizes differentiating hyponatremia subtypes, avoiding common diagnostic and therapeutic pitfalls, and optimizing patient care for individuals with cirrhosis complicated by hyponatremia.
Understanding Hyponatremia in Cirrhosis: Pathophysiology and Risk Factors
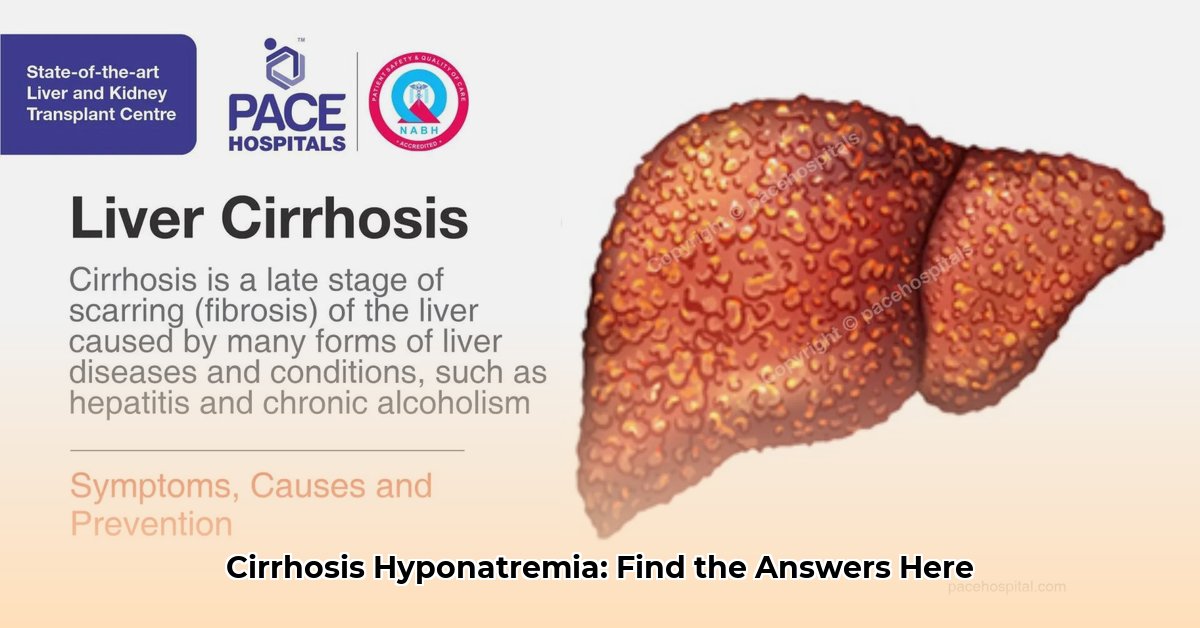
Cirrhosis, a progressive liver disease characterized by fibrosis and impaired liver function, frequently leads to hyponatremia (ICD-10 code E87.1). Hyponatremia represents a potentially life-threatening complication in patients with cirrhosis, underscoring the importance of recognizing the underlying mechanisms and risk factors to implement appropriate management strategies. The prevalence of hyponatremia in cirrhotic patients highlights the need for clinicians to maintain vigilance in monitoring sodium levels and to understand the implications of ICD-10 coding for accurate diagnosis and treatment tracking. The development of hyponatremia in cirrhosis involves a complex interplay of fluid imbalance, hormonal dysregulation, and impaired renal function, all contributing to the dilution of sodium in the extracellular fluid.
The Interplay of Cirrhosis and Hyponatremia
Cirrhosis disrupts the body’s delicate fluid balance, impairing the liver’s ability to regulate fluids, hormones, and kidney function. Hyponatremia arises as a consequence of this disruption, where the liver’s dysfunction leads to excessive water retention and subsequent dilution of sodium in the bloodstream. This dilution has profound implications, disrupting normal nerve and muscle function, thereby impacting physical and cognitive function. Restoring this equilibrium requires a multifaceted approach that addresses the underlying causes of fluid imbalance.
Unveiling the Science: Root Causes of Low Sodium
Several factors contribute to the development of hyponatremia in individuals with cirrhosis:
- Impaired Renal Water Excretion: Cirrhosis-associated complications, such as portal hypertension and splanchnic vasodilation, can lead to reduced effective circulating volume and activation of the renin-angiotensin-aldosterone system (RAAS) and increased secretion of antidiuretic hormone (ADH), also known as vasopressin. ADH promotes water reabsorption in the kidneys, contributing to dilutional hyponatremia.
- Dysregulation of Sodium and Water Balance: The RAAS and ADH play a critical role in regulating sodium and water balance. In cirrhosis, the overactivity of these hormonal systems leads to increased sodium and water retention, further exacerbating hyponatremia.
- Systemic Vasodilation: Cirrhosis-induced vasodilation, particularly in the splanchnic circulation, leads to a decrease in effective circulating volume, triggering the release of ADH and promoting water retention.
These interconnected factors make the regulation of sodium levels challenging, underscoring the importance of identifying the specific underlying mechanisms driving hyponatremia in each individual patient. Simply administering sodium supplements is often insufficient and can be harmful without addressing the root causes.
Classifying Hyponatremia: A Key to Effective Management
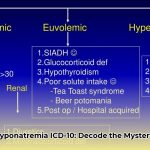
Hyponatremia can be classified based on serum osmolality and volume status, which guides diagnosis and treatment:
- Hypotonic Hyponatremia: The most common type, characterized by low serum osmolality (<275 mOsm/kg). It is further subdivided based on volume status:
- Hypovolemic Hyponatremia: Occurs with decreased total body water and sodium. This is often caused by diuretic overuse, gastrointestinal losses, or inadequate fluid intake.
- Euvolemic Hyponatremia: Characterized by normal total body water, but an excess relative to sodium. Common causes include Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH) and hypothyroidism.
- Hypervolemic Hyponatremia: Occurs with increased total body water and sodium, but water is in greater excess. This is typically seen in cirrhosis, heart failure, and nephrotic syndrome.
- Isotonic Hyponatremia: Serum osmolality is normal (275-295 mOsm/kg). This is also known as pseudohyponatremia and is often due to lab errors or elevated lipids or protein.
- Hypertonic Hyponatremia: Serum osmolality is high (>295 mOsm/kg). This is caused by the presence of osmotically active substances in the extracellular fluid, such as glucose in diabetic ketoacidosis or mannitol.
Differential Diagnosis: Identifying Hyponatremia in Cirrhosis
Diagnosing hyponatremia requires blood tests to measure sodium levels, but the real challenge lies in determining the underlying cause, particularly in patients with cirrhosis. Essential diagnostic steps include:
- Assessing Volume Status: Determining whether the patient is dehydrated (hypovolemic), euvolemic, or retaining excess fluid (hypervolemic) is critical, as it guides treatment strategies. Clinical assessment, including evaluation of blood pressure, heart rate, and edema, is essential.
- Measuring Serum Osmolality: Measuring serum osmolality is crucial to classify the type of hyponatremia (hypotonic, isotonic, or hypertonic).
- Evaluating Urine Osmolality and Sodium: Urine tests, specifically measuring urine osmolality and sodium concentration, provide valuable insights into kidney function and the underlying cause of hyponatremia. Low urine sodium suggests extrarenal losses, while high urine sodium suggests renal salt wasting or SIADH.
- Comprehensive Laboratory Evaluation: A complete laboratory evaluation is essential, including liver function tests, kidney function tests, serum electrolytes, and thyroid-stimulating hormone (TSH) to assess overall health and identify potential contributing factors.
- Medication Review: Clinicians should review the patient’s medication list to identify drugs that may contribute to hyponatremia, such as diuretics, NSAIDs, and certain antidepressants.
Tailored Treatment: Personalized Strategies for Managing Low Sodium
Effective treatment of hyponatremia in cirrhosis depends on the underlying cause, severity, and the patient’s volume status:
- Hypovolemic Hyponatremia (Dehydration): The primary treatment involves intravenous fluid replacement with isotonic saline solution (0.9% NaCl) to restore circulating volume and sodium levels. Close monitoring of sodium levels is essential to avoid overly rapid correction, which can lead to osmotic demyelination syndrome (ODS).
- Hypervolemic Hyponatremia (Fluid Overload): Treatment focuses on fluid restriction to reduce excess fluid volume, coupled with diuretics (loop diuretics, such as furosemide) to promote fluid excretion. In some cases, vasopressin receptor antagonists (vaptans) may be considered to block the effects of ADH, but their use requires careful monitoring due to potential liver toxicity.
- Euvolemic Hyponatremia: The treatment depends on the underlying cause, such as SIADH or hypothyroidism.
Treatment Strategies: At a Glance
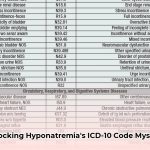
| Type of Hyponatremia | Main Treatment | Other Important Considerations |
|---|---|---|
| Hypovolemic (Dehydrated) | Fluid Replacement (IV Fluids, Isotonic Saline) | Close monitoring of sodium levels to avoid rapid correction; address the underlying cause of dehydration |
| Hypervolemic (Fluid Overload) | Fluid Restriction, Diuretics (Loop Diuretics) | Careful monitoring of electrolytes and fluid balance; consider vasopressin receptor antagonists (vaptans) with caution |
| Euvolemic | Treat underlying cause (SIADH, hypothyroidism, etc.) | Fluid restriction may be needed |
Prognosis and Long-Term Implications
Hyponatremia in cirrhosis patients often indicates advanced liver disease and is associated with a poorer prognosis and increased mortality risk. Hyponatremia can lead to various complications, including:
- Hepatic Encephalopathy: Hyponatremia can worsen hepatic encephalopathy, a neuropsychiatric complication of cirrhosis.
- Increased Risk of Infections: Hyponatremia has been linked to an increased risk of bacterial infections in cirrhotic patients.
- Increased Mortality: Numerous studies have demonstrated that hyponatremia is an independent predictor of mortality in patients with cirrhosis, both before and after liver transplantation.
Future Outlook: Research and Advancements
Ongoing research endeavors focus on:
- Development of improved diagnostic methods for early detection of hyponatremia and identification of underlying causes.
- Development of safer, more effective treatments for hyponatremia in cirrhosis, with a focus on personalized approaches.
- Identification of early warning signs and biomarkers for timely intervention and improved patient outcomes.
Effective management of hyponatremia in cirrhosis requires accurate diagnosis, personalized treatment strategies, and continued research to improve outcomes and quality of life for affected individuals.
Mastering Hypervolemic Hyponatremia Management in Cirrhosis
Key Insights:
- Hyponatremia is a common complication of cirrhosis, particularly the hypervolemic type.
- Accurate
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026